Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
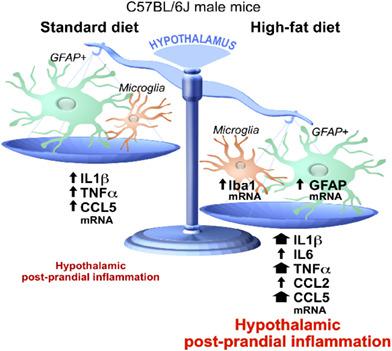
Dietary fat exacerbates postprandial hypothalamic inflammation involving glial fibrillary acidic protein-positive cells and microglia in male mice.
Glia ( IF 5.4 ) Pub Date : 2020-07-13 , DOI: 10.1002/glia.23882 Céline Cansell 1 , Katharina Stobbe 1 , Clara Sanchez 1 , Ophélia Le Thuc 1 , Coralie-Anne Mosser 2 , Selma Ben-Fradj 3 , Joris Leredde 1 , Cynthia Lebeaupin 1 , Delphine Debayle 1 , Lucile Fleuriot 1 , Frédéric Brau 1 , Nadège Devaux 1 , Alexandre Benani 3 , Etienne Audinat 4 , Nicolas Blondeau 1 , Jean-Louis Nahon 1 , Carole Rovère 1
Glia ( IF 5.4 ) Pub Date : 2020-07-13 , DOI: 10.1002/glia.23882 Céline Cansell 1 , Katharina Stobbe 1 , Clara Sanchez 1 , Ophélia Le Thuc 1 , Coralie-Anne Mosser 2 , Selma Ben-Fradj 3 , Joris Leredde 1 , Cynthia Lebeaupin 1 , Delphine Debayle 1 , Lucile Fleuriot 1 , Frédéric Brau 1 , Nadège Devaux 1 , Alexandre Benani 3 , Etienne Audinat 4 , Nicolas Blondeau 1 , Jean-Louis Nahon 1 , Carole Rovère 1
Affiliation
|
In humans, obesity is associated with brain inflammation, glial reactivity, and immune cells infiltration. Studies in rodents have shown that glial reactivity occurs within 24 hr of high‐fat diet (HFD) consumption, long before obesity development, and takes place mainly in the hypothalamus (HT), a crucial brain structure for controlling body weight. Here, we sought to characterize the postprandial HT inflammatory response to 1, 3, and 6 hr of exposure to either a standard diet (SD) or HFD. HFD exposure increased gene expression of astrocyte and microglial markers (glial fibrillary acidic protein [GFAP] and Iba1, respectively) compared to SD‐treated mice and induced morphological modifications of microglial cells in HT. This remodeling was associated with higher expression of inflammatory genes and differential regulation of hypothalamic neuropeptides involved in energy balance regulation. DREADD and PLX5622 technologies, used to modulate GFAP‐positive or microglial cells activity, respectively, showed that both glial cell types are involved in hypothalamic postprandial inflammation, with their own specific kinetics and reactiveness to ingested foods. Thus, recurrent exacerbated postprandial inflammation in the brain might promote obesity and needs to be characterized to address this worldwide crisis.
中文翻译:

膳食脂肪加剧了雄性小鼠中涉及胶质纤维酸性蛋白阳性细胞和小胶质细胞的餐后下丘脑炎症。
在人类中,肥胖与脑部炎症、神经胶质反应和免疫细胞浸润有关。对啮齿动物的研究表明,神经胶质反应发生在食用高脂饮食 (HFD) 的 24 小时内,远早于肥胖发展,并且主要发生在下丘脑 (HT) 中,这是控制体重的关键大脑结构。在这里,我们试图描述暴露于标准饮食 (SD) 或 HFD 1、3 和 6 小时后的餐后 HT 炎症反应。与 SD 处理的小鼠相比,HFD 暴露增加了星形胶质细胞和小胶质细胞标志物(分别为胶质纤维酸性蛋白 [GFAP] 和 Iba1)的基因表达,并诱导了 HT 中小胶质细胞的形态学改变。这种重塑与炎症基因的更高表达和参与能量平衡调节的下丘脑神经肽的差异调节有关。分别用于调节 GFAP 阳性或小胶质细胞活性的 DREADD 和 PLX5622 技术表明,两种胶质细胞类型都参与下丘脑餐后炎症,具有其自身特定的动力学和对摄入食物的反应性。因此,大脑中反复加剧的餐后炎症可能会促进肥胖,需要对其进行表征以解决这一全球性危机。具有自己特定的动力学和对摄入食物的反应性。因此,大脑中反复加剧的餐后炎症可能会促进肥胖,需要对其进行表征以解决这一全球性危机。具有自己特定的动力学和对摄入食物的反应性。因此,大脑中反复加剧的餐后炎症可能会促进肥胖,需要对其进行表征以解决这一全球性危机。
更新日期:2020-07-13
中文翻译:

膳食脂肪加剧了雄性小鼠中涉及胶质纤维酸性蛋白阳性细胞和小胶质细胞的餐后下丘脑炎症。
在人类中,肥胖与脑部炎症、神经胶质反应和免疫细胞浸润有关。对啮齿动物的研究表明,神经胶质反应发生在食用高脂饮食 (HFD) 的 24 小时内,远早于肥胖发展,并且主要发生在下丘脑 (HT) 中,这是控制体重的关键大脑结构。在这里,我们试图描述暴露于标准饮食 (SD) 或 HFD 1、3 和 6 小时后的餐后 HT 炎症反应。与 SD 处理的小鼠相比,HFD 暴露增加了星形胶质细胞和小胶质细胞标志物(分别为胶质纤维酸性蛋白 [GFAP] 和 Iba1)的基因表达,并诱导了 HT 中小胶质细胞的形态学改变。这种重塑与炎症基因的更高表达和参与能量平衡调节的下丘脑神经肽的差异调节有关。分别用于调节 GFAP 阳性或小胶质细胞活性的 DREADD 和 PLX5622 技术表明,两种胶质细胞类型都参与下丘脑餐后炎症,具有其自身特定的动力学和对摄入食物的反应性。因此,大脑中反复加剧的餐后炎症可能会促进肥胖,需要对其进行表征以解决这一全球性危机。具有自己特定的动力学和对摄入食物的反应性。因此,大脑中反复加剧的餐后炎症可能会促进肥胖,需要对其进行表征以解决这一全球性危机。具有自己特定的动力学和对摄入食物的反应性。因此,大脑中反复加剧的餐后炎症可能会促进肥胖,需要对其进行表征以解决这一全球性危机。











































 京公网安备 11010802027423号
京公网安备 11010802027423号