当前位置:
X-MOL 学术
›
J. Mater. Chem. B
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Mesenchymal stem cell-derived microvesicles mediate BMP2 gene delivery and enhance bone regeneration.
Journal of Materials Chemistry B ( IF 6.1 ) Pub Date : 2020-06-18 , DOI: 10.1039/d0tb00422g Zhuo Liang 1 , Yue Luo 1 , Yonggang Lv 1
Journal of Materials Chemistry B ( IF 6.1 ) Pub Date : 2020-06-18 , DOI: 10.1039/d0tb00422g Zhuo Liang 1 , Yue Luo 1 , Yonggang Lv 1
Affiliation
|
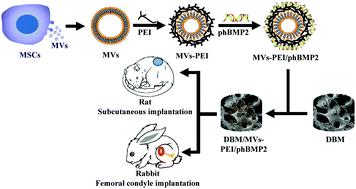
A demineralized bone matrix (DBM) scaffold has good biocompatibility, low antigenicity, a natural porous structure and no cytotoxicity, and so it is an appropriate material for bone regeneration. However, osteoinductive growth factors are often removed during preparation, which destroys the osteoinductive capacity of the DBM scaffold. Biomaterials combined with gene therapy is a promising approach to effectively avoid this adverse side effect. This study develops a human bone morphogenetic protein 2 (hBMP2) gene-activated DBM scaffold to enhance the osteoinductive capacity of DBM and improve bone repair. Bone marrow mesenchymal stem cell (MSC)-derived microvesicles (MVs) were obtained, and polyethyleneimine (PEI) and human bone morphogenetic protein 2 (hBMP2) plasmids (phBMP2) were sequentially coated on the MVs by layer-by-layer (LBL) self-assembly to form an MVs–PEI/phBMP2 non-viral gene vector. Finally, the gene-activated scaffold (DBM/MVs–PEI/phBMP2) was prepared by loading MVs–PEI/phBMP2 onto a DBM scaffold. The experimental results show that the MVs–PEI/phBMP2 exhibits higher transfection efficiency and lower cytotoxicity to MSCs when the MVs/PEI weight ratio = 5, and could enhance the osteogenic differentiation of MSCs in vitro. Subcutaneous implantation into rats showed that the DBM/MVs–PEI/phBMP2 scaffold could efficiently enhance the deposition of: collagen fibers, osteocalcin, osteopontin and CD34 endogenous proteins. Rabbit femoral condyle defect experiments proved that the DBM/MVs–PEI/phBMP2 scaffold could significantly promote bone repair. This study presents a novel, highly efficient and low cytotoxicity gene delivery vector based on MVs. The gene-activated DBM scaffold based on MVs not only could promote bone formation but also angiogenesis, implying that this kind of gene-activated scaffold is a promising bone substitute material.
中文翻译:

间充质干细胞来源的微泡介导BMP2基因的传递并增强骨再生。
脱矿骨基质(DBM)支架具有良好的生物相容性,低抗原性,天然的多孔结构且无细胞毒性,因此是骨骼再生的合适材料。然而,在制备过程中常常去除骨诱导生长因子,这破坏了DBM支架的骨诱导能力。生物材料与基因疗法相结合是有效避免这种不良副作用的有前途的方法。这项研究开发了人类骨形态发生蛋白2(hBMP2)基因激活的DBM支架,以增强DBM的骨诱导能力并改善骨修复。获得了骨髓间充质干细胞(MSC)衍生的微囊泡(MVs),聚乙烯亚胺(PEI)和人骨形态发生蛋白2(hBMP2)质粒(phBMP2)通过层层(LBL)自组装顺序包被在MV上,形成MVs-PEI / phBMP2非病毒基因载体。最后,通过将MVs-PEI / phBMP2加载到DBM支架上来制备基因激活的支架(DBM / MVs-PEI / phBMP2)。实验结果表明,当MVs / PEI重量比= 5时,MVs-PEI / phBMP2表现出更高的转染效率和对MSCs的细胞毒性,并且可以增强MSCs的成骨分化体外。皮下植入大鼠体内表明,DBM / MVs-PEI / phBMP2支架可以有效增强以下物质的沉积:胶原纤维,骨钙素,骨桥蛋白和CD34内源性蛋白质。兔股骨dy defect缺损实验证明,DBM / MVs-PEI / phBMP2支架可显着促进骨修复。这项研究提出了一种基于MVs的新型,高效,低细胞毒性基因传递载体。基于MVs的基因激活支架不仅可以促进骨形成,而且可以促进血管生成,这表明这种基因激活支架是一种很有前途的骨替代材料。
更新日期:2020-08-05
中文翻译:

间充质干细胞来源的微泡介导BMP2基因的传递并增强骨再生。
脱矿骨基质(DBM)支架具有良好的生物相容性,低抗原性,天然的多孔结构且无细胞毒性,因此是骨骼再生的合适材料。然而,在制备过程中常常去除骨诱导生长因子,这破坏了DBM支架的骨诱导能力。生物材料与基因疗法相结合是有效避免这种不良副作用的有前途的方法。这项研究开发了人类骨形态发生蛋白2(hBMP2)基因激活的DBM支架,以增强DBM的骨诱导能力并改善骨修复。获得了骨髓间充质干细胞(MSC)衍生的微囊泡(MVs),聚乙烯亚胺(PEI)和人骨形态发生蛋白2(hBMP2)质粒(phBMP2)通过层层(LBL)自组装顺序包被在MV上,形成MVs-PEI / phBMP2非病毒基因载体。最后,通过将MVs-PEI / phBMP2加载到DBM支架上来制备基因激活的支架(DBM / MVs-PEI / phBMP2)。实验结果表明,当MVs / PEI重量比= 5时,MVs-PEI / phBMP2表现出更高的转染效率和对MSCs的细胞毒性,并且可以增强MSCs的成骨分化体外。皮下植入大鼠体内表明,DBM / MVs-PEI / phBMP2支架可以有效增强以下物质的沉积:胶原纤维,骨钙素,骨桥蛋白和CD34内源性蛋白质。兔股骨dy defect缺损实验证明,DBM / MVs-PEI / phBMP2支架可显着促进骨修复。这项研究提出了一种基于MVs的新型,高效,低细胞毒性基因传递载体。基于MVs的基因激活支架不仅可以促进骨形成,而且可以促进血管生成,这表明这种基因激活支架是一种很有前途的骨替代材料。











































 京公网安备 11010802027423号
京公网安备 11010802027423号