JACC: Heart Failure ( IF 10.3 ) Pub Date : 2020-06-10 , DOI: 10.1016/j.jchf.2020.03.014 Eileen M Hsich 1 , Eugene H Blackstone 2 , Lucy W Thuita 3 , Dennis M McNamara 4 , Joseph G Rogers 5 , Clyde W Yancy 6 , Lee R Goldberg 7 , Maryam Valapour 8 , Gang Xu 9 , Hemant Ishwaran 10
|
Objectives
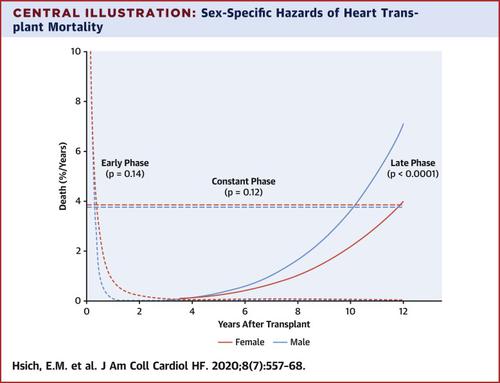
This study aims to understand the complex factors affecting heart transplant survival and to determine the importance of possible sex-specific risk factors.
Background
Heart transplant allocation is primarily focused on preventing waitlist mortality. To prevent organ wastage, future allocation must balance risk of waitlist mortality with post-transplantation mortality. However, more information regarding risk factors after heart transplantation is needed.
Methods
We included all adults (30,606) in the Scientific Registry of Transplant Recipients database who underwent isolated heart transplantation from January 1, 2004, to July 1, 2018. Mortality (8,278 deaths) was verified with the complete Social Security Death Index with a median follow-up of 3.9 years. Temporal decomposition was used to identify phases of survival and phase-specific risk factors. The random survival forests method was used to determine importance of mortality risk factors and their interactions.
Results
We identified 3 phases of mortality risk: early post-transplantation, constant, and late. Sex was not a significant risk factor. There were several interactions predicting early mortality such as pretransplantation mechanical ventilation with presence of end-organ function (bilirubin, renal function) and interactions predicting later mortality such as diabetes and older age (donor and recipient). More complex interactions predicting early-, mid-, and late-mortality existed and were identified with machine learning (i.e., elevated bilirubin, mechanical ventilation, and dialysis).
Conclusions
Post–heart transplant mortality risk is complex and dynamic, changing with time and events. Sex is not an important mortality risk factor. To prevent organ wastage, end-organ dysfunction should be resolved before transplantation as much as possible.
中文翻译:

心脏移植:深度生存分析。
目标
这项研究旨在了解影响心脏移植生存的复杂因素,并确定可能的性别特异性危险因素的重要性。
背景
心脏移植的分配主要集中在预防候补名单死亡率上。为了防止器官浪费,未来的分配必须在等待名单死亡率与移植后死亡率之间进行权衡。但是,需要更多有关心脏移植后危险因素的信息。
方法
我们将所有2004年1月1日至2018年7月1日接受孤立心脏移植的成年人(30,606)纳入了移植接受者科学注册数据库。死亡率(8,278例死亡)已通过完整的社会保障死亡指数进行了核实,中位数如下3.9年 时间分解被用来识别生存阶段和特定阶段的危险因素。随机生存森林方法用于确定死亡率危险因素及其相互作用的重要性。
结果
我们确定了死亡风险的三个阶段:移植后早期,持续和晚期。性不是重要的危险因素。有多种相互作用可预测早期死亡率,例如移植前机械通气伴有终末器官功能(胆红素,肾功能),以及相互作用可预测晚期死亡率,例如糖尿病和老年(供体和受体)。存在更复杂的相互作用,可以预测早期,中期和晚期死亡,并且已通过机器学习进行了识别(例如,胆红素升高,机械通气和透析)。
结论
心脏移植后的死亡风险复杂而动态,随时间和事件而变化。性别不是重要的死亡风险因素。为防止器官浪费,应在移植前尽可能解决终末器官功能障碍。











































 京公网安备 11010802027423号
京公网安备 11010802027423号