JACC: Heart Failure ( IF 10.3 ) Pub Date : 2020-06-10 , DOI: 10.1016/j.jchf.2020.03.009 Wendy McCallum 1 , Hocine Tighiouart 2 , Jeffrey M Testani 3 , Matthew Griffin 3 , Marvin A Konstam 4 , James E Udelson 4 , Mark J Sarnak 1
|
Objectives
This study aimed to examine whether incorporation of a comprehensive set of measures of decongestion modifies the association of acute declines in kidney function with outcomes.
Background
In-hospital acute declines in kidney function occur in approximately 20% to 30% of patients admitted with acute decompensated heart failure (ADHF) and may be associated with adverse outcomes.
Methods
Using data from EVEREST (Efficacy of Vasopressin Antagonism in Heart Failure Outcome Study With Tolvaptan), we used multivariable Cox regression models to evaluate the association between in-hospital changes in estimated glomerular filtration rate (eGFR) with death and a composite outcome of cardiovascular death and hospitalization for heart failure. We evaluated eGFR declines within the context of changes in markers of volume overload including b-type natriuretic peptide (BNP), N-terminal prohormone of B-type natriuretic peptide (NT-proBNP), and weight, as well as changes in measures of hemoconcentration including hematocrit, albumin, and total protein.
Results
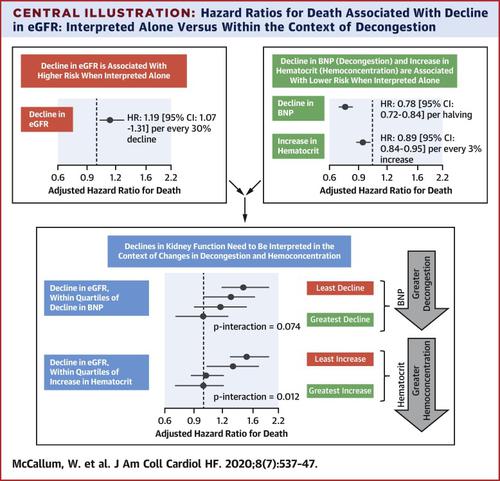
Among 3,715 patients over a median follow-up of 9.9 months, every 30% decline in eGFR was associated with higher risk of both death (hazard ratio [HR]: 1.19; 95% confidence interval [CI]: 1.07 to 1.31) and the composite outcome (HR: 1.09; 95% CI: 1.01 to 1.18) in adjusted models. The acute decline in eGFR was no longer associated with higher risk of either outcome as long as there was evidence of decongestion, either by declines in BNP, NT-proBNP, or weight or by increases in hematocrit, albumin or total protein. Interaction testing between decline in eGFR and changes in hematocrit, albumin, and total protein was statistically significant (p interaction of <0.01 for death and p interaction of ≤0.01 for composite for all 3 biomarkers). Interaction between change in eGFR and changes in BNP (p interaction = 0.07 for death; p interaction = 0.08 for composite), NT-proBNP (p interaction = 0.15 for death; p interaction = 0.18 for composite) and weight (p interaction = 0.13 for death; p interaction = 0.19 for composite) did not meet statistical significance.
Conclusions
Overall, acute declines in eGFR are associated with adverse outcomes, with evidence of modification by changes in markers of decongestion, suggesting that they are no longer associated with adverse outcomes if these markers are concomitantly improving.
中文翻译:

在急性失代偿性心力衰竭减充血的情况下,急性肾功能下降。
目标
本研究旨在检验综合一套减轻充血的措施是否会改变肾功能急性下降与结果的关联。
背景
大约 20% 至 30% 的急性失代偿性心力衰竭 (ADHF) 入院患者发生院内肾功能急性下降,这可能与不良结局有关。
方法
使用来自 EVEREST(托伐普坦在心力衰竭结果研究中血管加压素拮抗作用的疗效)的数据,我们使用多变量 Cox 回归模型来评估估计肾小球滤过率 (eGFR) 的院内变化与死亡和心血管死亡的复合结果之间的关联和因心力衰竭住院。我们评估了容量超负荷标志物(包括 b 型利钠肽 (BNP)、B 型利钠肽的 N 末端激素原 (NT-proBNP) 和体重)的变化以及体重的变化背景下的 eGFR 下降。血液浓度包括血细胞比容、白蛋白和总蛋白。
结果
在中位随访时间为 9.9 个月的 3,715 名患者中,eGFR 每下降 30% 与更高的死亡风险相关(风险比 [HR]:1.19;95% 置信区间 [CI]:1.07 至 1.31)和调整模型中的复合结果(HR:1.09;95% CI:1.01 至 1.18)。只要有减轻充血的证据,无论是通过 BNP、NT-proBNP 或体重的下降,还是通过红细胞比容、白蛋白或总蛋白的增加,eGFR 的急剧下降不再与任一结局的较高风险相关。eGFR 下降与血细胞比容、白蛋白和总蛋白变化之间的相互作用测试具有统计学意义(对于所有 3 种生物标志物,死亡的 p 相互作用 <0.01,复合物的 p 相互作用≤0.01)。eGFR 变化与 BNP 变化之间的相互作用(p 相互作用 = 0.07 死亡;p 相互作用 = 0。
结论
总体而言,eGFR 的急剧下降与不良结果相关,有证据表明减轻充血标志物的变化会有所改变,这表明如果这些标志物同时改善,则它们不再与不良结果相关。











































 京公网安备 11010802027423号
京公网安备 11010802027423号