Gastrointestinal Endoscopy ( IF 6.7 ) Pub Date : 2020-06-09 , DOI: 10.1016/j.gie.2020.05.061 Anna Tavakkoli 1 , B Joseph Elmunzer 2 , Akbar K Waljee 3 , Caitlin C Murphy 4 , Sandi L Pruitt 4 , Hong Zhu 4 , Rong Rong 5 , Richard S Kwon 6 , James M Scheiman 7 , Joel H Rubenstein 8 , Amit G Singal 1
|
Background and Aims
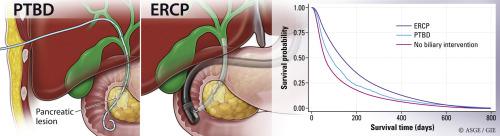
Most patients with pancreatic cancer are diagnosed at a late stage and are not candidates for surgical resection. Many have jaundice requiring biliary drainage, which can be accomplished using ERCP or percutaneous transhepatic biliary drainage (PTBD). To date, no studies have evaluated the impact of ERCP or PTBD on survival among patients with unresectable pancreatic cancer. The aims of our study were to compare overall survival between patients with unresectable pancreatic cancer receiving ERCP with those receiving PTBD, to compare overall survival between patients who received a biliary intervention (ERCP or PTBD) versus those who received no biliary intervention, and to compare secondary outcomes, such as length of hospital stay and costs, between ERCP and PTBD.
Methods
We conducted a retrospective cohort study using the Surveillance, Epidemiology, and End Results–Medicare database. Patients with known pancreatic cancer were included if they had a pancreatic head mass and/or evidence of biliary obstruction. We used a time-varying Cox proportional hazards model to estimate overall survival of patients receiving ERCP versus PTBD and overall survival among patients who received a biliary intervention versus no biliary drainage. Secondary outcomes included length of hospital stay, costs, and admissions within 30 days.
Results
Of 14,808 patients with unresectable pancreatic cancer, 8898 patients (60.0%) underwent biliary drainage and 5910 patients (39.9%) received no biliary intervention. ERCP accounted for most biliary interventions (8271, 93.0%), whereas 623 patients (7.0%) underwent PTBD. In multivariable analysis, ERCP was associated with reduced mortality compared with PTBD (adjusted hazard ratio [aHR], .67; 95% confidence interval [CI], .60-.75). When ERCP or PTBD was compared with no biliary intervention, both procedures were associated with a survival benefit (aHR, .51 [95% CI, .49-.54] and .53 [95% CI, .48-.59], respectively). Compared with patients receiving PTBD, those who underwent ERCP had shorter mean length of hospital stay (7.0 ± 5.7 days vs 9.6 ± 6.6 days, respectively; P < .001) and lower hospital charges ($54,899.25 vs $75,246.00, P < .001) but no significant difference in hospitalization or 30-day readmissions.
Conclusions
ERCP is associated with reduced mortality compared with PTBD in pancreatic cancer patients, highlighting the critical role of ERCP in the management of biliary obstruction from pancreatic cancer.
中文翻译:

不可切除的胰腺癌患者接受内镜或经皮介入治疗的生存分析。
背景和目标
大多数胰腺癌患者被诊断为晚期,不适合手术切除。许多人患有需要胆道引流的黄疸,这可以使用 ERCP 或经皮经肝胆道引流 (PTBD) 来完成。迄今为止,还没有研究评估 ERCP 或 PTBD 对不可切除胰腺癌患者生存的影响。我们研究的目的是比较接受 ERCP 与接受 PTBD 的不可切除胰腺癌患者的总生存期,比较接受胆道干预(ERCP 或 PTBD)与未接受胆道干预的患者之间的总生存期,并比较ERCP 和 PTBD 之间的次要结果,例如住院时间和费用。
方法
我们使用监测、流行病学和最终结果-医疗保险数据库进行了一项回顾性队列研究。如果患者有胰头肿块和/或胆道梗阻证据,则纳入已知胰腺癌患者。我们使用时变 Cox 比例风险模型来估计接受 ERCP 与 PTBD 患者的总生存期以及接受胆道干预与无胆道引流患者的总生存期。次要结果包括住院时间、费用和 30 天内的入院情况。
结果
在 14808 例不可切除胰腺癌患者中,8898 例(60.0%)接受了胆道引流,5910 例(39.9%)未接受胆道介入治疗。ERCP 占大多数胆道干预 (8271, 93.0%),而 623 名患者 (7.0%) 接受了 PTBD。在多变量分析中,与 PTBD 相比,ERCP 与死亡率降低相关(调整后的风险比 [aHR],0.67;95% 置信区间 [CI],0.60-.75)。当 ERCP 或 PTBD 与无胆道干预进行比较时,两种手术都与生存获益相关(aHR,0.51 [95% CI,0.49-.54] 和 0.53 [95% CI,0.48-.59],分别)。与接受 PTBD 的患者相比,接受 ERCP 的患者平均住院时间更短(分别为 7.0 ± 5.7 天和 9.6 ± 6.6 天;P < .001)和较低的住院费用(54,899.25 美元对比 75,246.00 美元,P < .001),但住院或 30 天再入院率没有显着差异。
结论
与胰腺癌患者的 PTBD 相比,ERCP 与降低死亡率相关,突出了 ERCP 在胰腺癌胆道梗阻管理中的关键作用。











































 京公网安备 11010802027423号
京公网安备 11010802027423号