Journal of the American College of Surgeons ( IF 3.8 ) Pub Date : 2020-05-15 , DOI: 10.1016/j.jamcollsurg.2020.05.005 Mark J Truty 1 , Jill J Colglazier 2 , Bernardo C Mendes 2 , David M Nagorney 1 , Thomas C Bower 2 , Rory L Smoot 1 , Randall R DeMartino 2 , Sean P Cleary 1 , Gustavo S Oderich 2 , Michael L Kendrick 1
|
Background
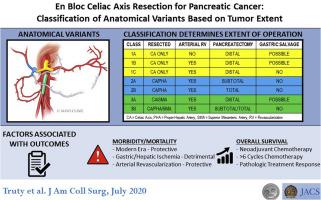
En bloc celiac axis resection (CAR) for pancreatic cancer is considered increasingly after modern neoadjuvant chemotherapy (NAC). Appleby and distal pancreatectomy with CAR are anatomically inaccurate terms, as tumors can extend beyond celiac axis proper, requiring concurrent resection of the proper hepatic artery and/or superior mesenteric artery.
Study Design
A 3-level classification for CAR (class 1, 2, or 3) was developed after retrospective review of an arterial resection database describing anatomical variants that dictate pancreatectomy-type, formal arterial revascularization, and gastric preservation. Perioperative and oncologic outcomes were assessed.
Results
Of 90 CARs for pancreatic cancer, 89% patients received NAC, 35% requiring chemotherapeutic switch. There were 41 class 1, 33 class 2, and 16 class 3 CARs, with arterial and venous revascularization performed 62% and 66%, respectively. Ninety-day mortality decreased to 4% in the last 50 cases (p = 0.035); major morbidity was unchanged (55%). Any hepatic or gastric ischemia occurred in 20% and 10% patients, respectively, and arterial revascularization was protective. R0 resection rate (88%) was associated with chemoradiation (p = 0.004). Median overall survival was 36.2 months, superior with NAC (8.0 vs. 43.5 months). Predictors of survival after NAC included chemotherapy duration, carbohydrate antigen 19-9 response, pathologic response, and lymph node status. Major pathologic response (p = 0.036) and extended duration NAC (p = 0.007) were independent predictors on multivariate analysis.
Conclusions
Current terminology for CAR inadequately describes all operative variants. Our classification, based on the largest single-center series, allows complex operative planning and standardized reporting across institutions. Extent of arterial involvement determines pancreatectomy type, need for arterial revascularization, and likelihood of gastric preservation. Operative mortality has improved, morbidity remains significant, and survival favorable after extended NAC with associated pathologic responses; given these factors, CAR should only be considered in fit patients with objective NAC responses at specialized centers.
中文翻译:

胰腺癌的腹腔全切除术:基于肿瘤范围的解剖学变异分类。
背景
现代新辅助化疗(NAC)后,胰腺癌的整体腹腔轴切除术(CAR)越来越多。Appleby手术和远端CAR胰腺切除术在解剖学上是不准确的术语,因为肿瘤可能会延伸到腹腔适当的轴外,因此需要同时切除适当的肝动脉和/或肠系膜上动脉。
学习规划
对动脉切除数据库进行回顾性研究后,制定了CAR的3级分类(1、2或3级),该数据库描述了指示胰腺切除术类型,正规动脉血运重建和胃保存的解剖变异。评估围手术期和肿瘤学结局。
结果
在90例胰腺癌CAR中,有89%的患者接受了NAC,其中35%的患者需要进行化学治疗。有1类41类,33类2类和16类3类CAR,分别进行了62%和66%的动脉和静脉血运重建。最近50例患者的90天死亡率降低到4%(p = 0.035);主要发病率未改变(55%)。任何肝或胃缺血分别发生在20%和10%的患者中,动脉血运重建具有保护作用。R0切除率(88%)与化学放疗相关(p = 0.004)。中位总生存期为36.2个月,NAC优于中位生存期(8.0对43.5个月)。NAC后存活的预测因素包括化疗持续时间,碳水化合物抗原19-9反应,病理反应和淋巴结状态。主要病理反应(p = 0.036)和持续时间NAC(p = 0。
结论
当前的CAR术语不足以描述所有可操作的变体。我们基于最大的单中心系列分类,可以进行复杂的运营计划和跨机构的标准化报告。动脉受累程度决定了胰腺切除术的类型,是否需要进行动脉血运重建以及胃保留的可能性。延长NAC并伴有相关病理反应后,手术死亡率有所提高,发病率仍然很高,并且生存期有利。考虑到这些因素,仅应在专门中心对具有客观NAC反应的合适患者考虑CAR。











































 京公网安备 11010802027423号
京公网安备 11010802027423号