Journal of the American College of Surgeons ( IF 3.8 ) Pub Date : 2020-05-15 , DOI: 10.1016/j.jamcollsurg.2020.05.006 Jason M Samuels 1 , Heather Carmichael 1 , Alexandra Kovar 1 , Shane Urban 2 , Stephanie Vega 2 , Catherine Velopulos 1 , Robert C McIntyre 1
|
Background
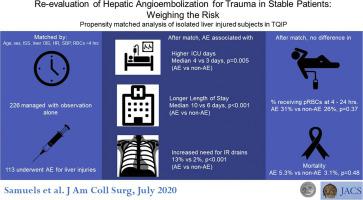
Angioembolization (AE) is recommended for extravasation from liver injury on CT. Data supporting AE are limited to retrospective series that have found low mortality but high morbidity. These studies did not focus on stable patients. We hypothesized that AE is associated with increased complications without improving mortality in stable patients.
Study Design
We queried the 2016 Trauma Quality Improvement Project database for patients with grade III or higher liver injury (Organ Injury Score ≥ 3), blunt mechanism, with stable vitals (systolic blood pressure ≥ 90 mmHg and heart rate of 50 to 110 beats/min). Exclusion criteria were nonhepatic intra-abdominal or pelvic injury (Organ Injury Score ≥ 3), laparotomy less than 6 hours, and AE implementation more than 24 hours. Patients were matched 1:2 (AE to non-AE) on age, sex, Injury Severity Score, liver Organ Injury Score, arrival systolic blood pressure and heart rate, and transfusion in the first 4 hours using propensity score logistic modeling. Primary outcomes were in-hospital mortality, length of stay, transfusion, hepatic resection, interventional radiology drainage, and endoscopic procedure.
Results
There were 1,939 patients who met criteria, with 116 (6%) undergoing hepatic AE. Median time to embolization was 3.3 hours. After successfully matching on all variables, groups did not differ with respect to mortality (5.4% vs 3.2%; p = 0.5, AE vs non-AE, respectively) or transfusion at 4 to 24 hours (4.4% vs 7.5%; p = 0.4). A larger percentage of the AE group underwent interventional radiology drainage (13.3% vs 2.2%; p < 0.001), with more ICU days (4 vs 3 days; p = 0.005) and longer length of stay (10 vs 6 days; p < 0.001).
Conclusions
Hepatic AE was associated with increased morbidity without improving mortality, suggesting the benefits of AE do not outweigh the risks in stable liver injury. Observing these patients is likely a more prudent approach.
中文翻译:

重新评估稳定患者的肝血管栓塞治疗的创伤:权衡风险。
背景
建议将血管栓塞(AE)用于CT上肝损伤的渗出。支持AE的数据仅限于回顾性系列,这些系列发现了低死亡率但高发病率。这些研究没有针对稳定的患者。我们假设AE与稳定的患者中增加的并发症而不增加死亡率相关。
学习规划
我们查询了2016年创伤质量改善项目数据库,该数据库针对三级或以上肝损伤(器官损伤评分≥3),机制钝,生命体征稳定(收缩压≥90 mmHg,心率50至110次/分钟)的患者。排除标准为非肝腹内或骨盆损伤(器官损伤评分≥3),剖腹手术少于6小时,AE实施超过24小时。使用倾向性得分逻辑模型在年龄,性别,损伤严重程度评分,肝器官损伤评分,到达收缩压和心率以及输血的最初4小时内对患者进行1:2(AE与非AE)匹配。主要结局为院内死亡率,住院时间,输血,肝切除,放射介入介入和内窥镜检查。
结果
有1939例符合标准的患者,其中116例(6%)进行了肝AE。栓塞的中位时间为3.3小时。在成功匹配所有变量后,各组的死亡率(分别为5.4%vs 3.2%; p = 0.5,AE与非AE)或4至24小时输血(4.4%vs 7.5%; p = 0.4)。AE组中有较大比例的患者接受了介入放射引流术(13.3%vs 2.2%; p <0.001),ICU天数更多(4 vs 3天; p = 0.005),住院时间更长(10 vs 6天; p < 0.001)。
结论
肝AE与发病率增加相关,但并未改善死亡率,这表明AE的益处并未超过稳定肝损伤的风险。观察这些患者可能是更谨慎的方法。











































 京公网安备 11010802027423号
京公网安备 11010802027423号