当前位置:
X-MOL 学术
›
JACC Heart Fail.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Assessment of HF Outcomes Using a Claims-Based Frailty Index.
JACC: Heart Failure ( IF 10.3 ) Pub Date : 2020-05-06 , DOI: 10.1016/j.jchf.2019.12.012 Sukruth A Shashikumar 1 , Alina A Luke 1 , Kenton J Johnston 2 , Karen E Joynt Maddox 3
JACC: Heart Failure ( IF 10.3 ) Pub Date : 2020-05-06 , DOI: 10.1016/j.jchf.2019.12.012 Sukruth A Shashikumar 1 , Alina A Luke 1 , Kenton J Johnston 2 , Karen E Joynt Maddox 3
Affiliation
|
OBJECTIVES
This study used a claims-based frailty index to investigate outcomes of frail patients with heart failure (HF).
BACKGROUND
Medicare value-based payment programs financially reward and penalize hospitals based on HF patients' outcomes. Although programs adjust risks for comorbidities, they do not adjust for frailty. Hospitals caring for high proportions of frail patients may be unfairly penalized. Understanding frail HF patients' outcomes may allow improved risk adjustment and more equitable assessment of health care systems.
METHODS
Adapting a claims-based frailty index, the study assigned a frailty score to each adult in the National in-patient Sample (NIS) from 2012 through September 2015 with a primary diagnosis of HF and dichotomized frailty by using a cutoff value established in the general NIS population. Multivariate regression models were estimated, controlling for comorbidities and hospital characteristics, to investigate relationships between frailty and outcomes.
RESULTS
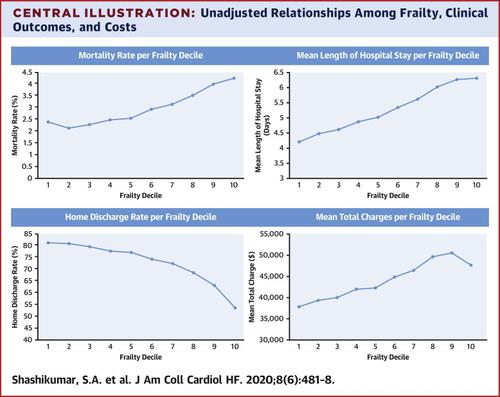
Of 732,932 patients, 369,298 were frail. Frail patients were more likely than nonfrail patients to die during hospital stay (3.57% vs. 2.37%, respectively; adjusted odds ratio [aOR]: 1.67; 95% confidence interval [CI]: 1.61 to 1.72; p < 0.001); were less likely to be discharged to home (66.5% vs. 79.3%, respectively; aOR: 0.58; 95% CI: 0.57 to 0.58; p < 0.001); were hospitalized for more days (5.89 vs. 4.63 days, respectively; adjusted coefficient: 0.21 days; 95% CI: 0.21 to 0.22; p < 0.001); and incurred higher charges ($47,651 vs. $40,173, respectively; adjusted difference = $9,006; 95% CI: $8,596 to $9,416; p < 0.001).
CONCLUSIONS
Frail patients with HF had significantly poorer outcomes than nonfrail patients after accounting for comorbidities. Clinicians should screen for frailty to identify high-risk patients who could benefit from targeted intervention. Policymakers should perform risk adjustments for frailty for more equitable quality measurement and financial incentive allocation.
中文翻译:

使用基于索赔的脆弱指数评估HF结果。
目的这项研究使用了基于索赔的脆弱指数来调查脆弱的心力衰竭(HF)患者的预后。背景技术基于医疗保险基于价值的支付程序基于HF患者的结果在经济上奖励和惩罚医院。尽管计划调整了合并症的风险,但并未针对脆弱性进行调整。照顾高比例脆弱患者的医院可能会受到不公平的惩罚。了解脆弱的HF患者的预后可能会改善风险调整并更公平地评估医疗保健系统。方法采用基于索赔的脆弱性指数,该研究为2012年至2015年9月的全国住院患者样本(NIS)中的每个成年人分配了脆弱性评分,并通过在研究中建立的临界值对HF和二分脆弱性进行了初步诊断。 NIS的一般人口。估计了多元回归模型,以控制合并症和医院特征,以研究虚弱与结局之间的关系。结果在732,932名患者中,有369,298名虚弱。体弱患者比非体弱患者在住院期间死亡的可能性更高(分别为3.57%和2.37%;调整后的优势比[aOR]:1.67; 95%置信区间[CI]:1.61至1.72; p <0.001);出院的可能性较小(分别为66.5%和79.3%; aOR:0.58; 95%CI:0.57至0.58; p <0.001);住院时间更长(分别为5.89和4.63天;调整系数:0.21天; 95%CI:0.21至0.22; p <0.001);并产生更高的费用(分别为47,651美元和40,173美元;调整后的差额= 9,006美元; 95%CI:8,596美元至9,416美元; p <0.001)。结论考虑到合并症后,体弱的HF患者的结局明显比非体弱的患者差。临床医生应筛选虚弱体质,以找出可以从目标干预中受益的高危患者。决策者应针对脆弱性进行风险调整,以实现更公平的质量衡量和财务激励分配。
更新日期:2020-05-06
中文翻译:

使用基于索赔的脆弱指数评估HF结果。
目的这项研究使用了基于索赔的脆弱指数来调查脆弱的心力衰竭(HF)患者的预后。背景技术基于医疗保险基于价值的支付程序基于HF患者的结果在经济上奖励和惩罚医院。尽管计划调整了合并症的风险,但并未针对脆弱性进行调整。照顾高比例脆弱患者的医院可能会受到不公平的惩罚。了解脆弱的HF患者的预后可能会改善风险调整并更公平地评估医疗保健系统。方法采用基于索赔的脆弱性指数,该研究为2012年至2015年9月的全国住院患者样本(NIS)中的每个成年人分配了脆弱性评分,并通过在研究中建立的临界值对HF和二分脆弱性进行了初步诊断。 NIS的一般人口。估计了多元回归模型,以控制合并症和医院特征,以研究虚弱与结局之间的关系。结果在732,932名患者中,有369,298名虚弱。体弱患者比非体弱患者在住院期间死亡的可能性更高(分别为3.57%和2.37%;调整后的优势比[aOR]:1.67; 95%置信区间[CI]:1.61至1.72; p <0.001);出院的可能性较小(分别为66.5%和79.3%; aOR:0.58; 95%CI:0.57至0.58; p <0.001);住院时间更长(分别为5.89和4.63天;调整系数:0.21天; 95%CI:0.21至0.22; p <0.001);并产生更高的费用(分别为47,651美元和40,173美元;调整后的差额= 9,006美元; 95%CI:8,596美元至9,416美元; p <0.001)。结论考虑到合并症后,体弱的HF患者的结局明显比非体弱的患者差。临床医生应筛选虚弱体质,以找出可以从目标干预中受益的高危患者。决策者应针对脆弱性进行风险调整,以实现更公平的质量衡量和财务激励分配。











































 京公网安备 11010802027423号
京公网安备 11010802027423号