JACC: Heart Failure ( IF 10.3 ) Pub Date : 2020-04-08 , DOI: 10.1016/j.jchf.2019.12.007 Sebhat Erqou 1 , Lan Jiang 2 , Gaurav Choudhary 1 , Michelle Lally 1 , Gerald S Bloomfield 3 , Andrew R Zullo 4 , Theresa I Shireman 5 , Mathew Freiberg 6 , Amy C Justice 7 , James Rudolph 8 , Nina Lin 9 , Wen-Chih Wu 1
|
Objectives
This study sought to investigate outcomes of heart failure (HF) in veterans living with human immunodeficiency virus (HIV).
Background
Data on outcomes of HF among people living with human immunodeficiency virus (PLHIV) are limited.
Methods
We performed a retrospective cohort study of Veterans Health Affairs data to investigate outcomes of HF in PLHIV. We identified 5,747 HIV+ veterans with diagnosis of HF from 2000 to 2018 and 33,497 HIV− frequency-matched controls were included. Clinical outcomes included all-cause mortality, HF hospital admission, and all-cause hospital admission.
Results
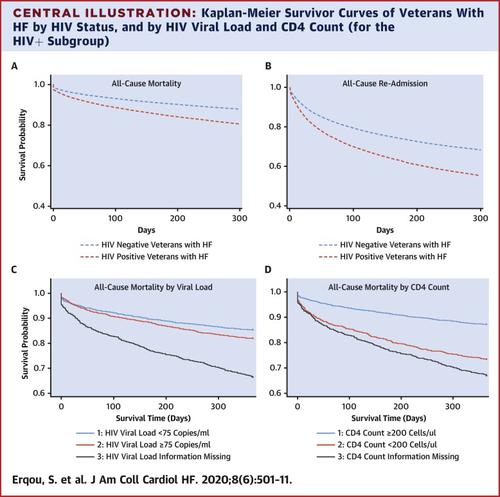
Compared with HIV− veterans with HF, HIV+ veterans with HF were more likely to be black (56% vs. 14%), be smokers (52% vs. 29%), use alcohol (32% vs. 13%) or drugs (37% vs. 8%), and have a higher comorbidity burden (Elixhauser comorbidity index 5.1 vs. 2.6). The mean ejection fraction (EF) (45 ± 16%) was comparable between HIV+ and HIV− veterans. HIV+ veterans with HF had a higher age-, sex-, and race-adjusted 1-year all-cause mortality (30.7% vs. 20.3%), HF hospital admission (21.2% vs. 18.0%), and all-cause admission (50.2% vs. 38.5%) rates. Among veterans with HIV and HF, those with low CD4 count (<200 cells/ml) and high HIV viral load (>75 copies/μl) had worse outcomes. The associations remained statistically significant after adjusting for extensive list of covariates. The incidence of all-cause mortality and HF admissions was higher among HIV+ veterans with ejection fraction <45%
Conclusions
HIV+ veterans with HF had higher risk of hospitalization and mortality compared with their HIV− counterparts, with worse outcomes reported for individuals with lower CD4 count, higher viral load, and lower ejection fraction.
中文翻译:

人类免疫缺陷病毒感染退伍军人的心力衰竭结果和相关因素。
目标
本研究旨在调查感染人类免疫缺陷病毒 (HIV) 的退伍军人心力衰竭 (HF) 的结果。
背景
人类免疫缺陷病毒 (PLHIV) 感染者的 HF 结局数据有限。
方法
我们对退伍军人健康事务数据进行了一项回顾性队列研究,以调查 HF 在 PLHIV 中的结果。从 2000 年到 2018 年,我们确定了 5,747 名 HIV+ 退伍军人被诊断为 HF,其中包括 33,497 名 HIV- 频率匹配的对照。临床结果包括全因死亡率、心衰住院和全因住院。
结果
与患有心力衰竭的 HIV- 退伍军人相比,患有心力衰竭的 HIV+ 退伍军人更有可能是黑人(56% 对 14%)、吸烟者(52% 对 29%)、饮酒(32% 对 13%)或吸毒(37% 对 8%),并有更高的合并症负担(Elixhauser 合并症指数 5.1 对 2.6)。HIV+ 和 HIV- 退伍军人的平均射血分数 (EF) (45 ± 16%) 相当。患有 HF 的 HIV+ 退伍军人具有更高的年龄、性别和种族调整后的 1 年全因死亡率(30.7% 对 20.3%)、HF 住院(21.2% 对 18.0%)和全因住院(50.2% 对 38.5%)率。在患有 HIV 和 HF 的退伍军人中,CD4 计数低(<200 个细胞/ml)和 HIV 病毒载量高(>75 拷贝/μl)的人预后较差。在调整了广泛的协变量列表后,这些关联仍然具有统计学意义。
结论
与 HIV- 患者相比,患有 HF 的 HIV+ 退伍军人住院和死亡的风险更高,据报道,CD4 计数较低、病毒载量较高和射血分数较低的个体的结局更差。











































 京公网安备 11010802027423号
京公网安备 11010802027423号