当前位置:
X-MOL 学术
›
Ann. N. Y. Acad. Sci.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Myeloid cells in sepsis-acquired immunodeficiency
Annals of the New York Academy of Sciences ( IF 4.1 ) Pub Date : 2020-03-23 , DOI: 10.1111/nyas.14333 Fabienne Venet 1, 2 , Julie Demaret 3 , Morgane Gossez 1, 2 , Guillaume Monneret 1, 2
Annals of the New York Academy of Sciences ( IF 4.1 ) Pub Date : 2020-03-23 , DOI: 10.1111/nyas.14333 Fabienne Venet 1, 2 , Julie Demaret 3 , Morgane Gossez 1, 2 , Guillaume Monneret 1, 2
Affiliation
|
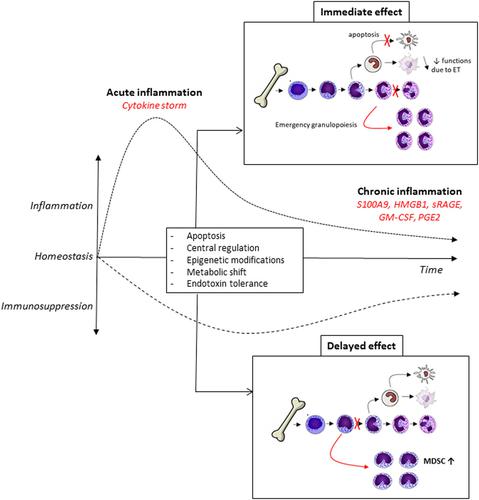
On May 2017, the World Health Organization recognized sepsis as a global health priority. Sepsis profoundly perturbs immune homeostasis by initiating a complex response that varies over time, with the concomitant occurrence of pro- and anti-inflammatory mechanisms. Sepsis deeply impacts myeloid cell response. Different mechanisms are at play, such as apoptosis, endotoxin tolerance, metabolic failure, epigenetic reprogramming, and central regulation. This induces systemic effects on circulating immune cells and impacts progenitors locally in lymphoid organs. In the bone marrow, a progressive shift toward the release of immature myeloid cells (including myeloid-derived suppressor cells), at the expense of mature neutrophils, takes place. Circulating dendritic cell number remains dramatically low and monocytes/macrophages display an anti-inflammatory phenotype and reduced antigen presentation capacity. Intensity and persistence of these alterations are associated with increased risk of deleterious outcomes in patients. Thus, myeloid cells dysfunctions play a prominent role in the occurrence of sepsis-acquired immunodeficiency. For the most immunosuppressed patients, this paves the way for clinical trials evaluating immunoadjuvant molecules (granulocyte-macrophage colony-stimulating factor and interferon gamma) aimed at restoring homeostatic myeloid cell response. Our review offers a summary of sepsis-induced myeloid cell dysfunctions and current therapeutic strategies proposed to target these defects in patients.
中文翻译:

脓毒症获得性免疫缺陷中的髓样细胞
2017 年 5 月,世界卫生组织将败血症确认为全球卫生重点。脓毒症通过引发随时间变化的复杂反应,伴随着促炎和抗炎机制的发生,严重扰乱了免疫稳态。脓毒症严重影响骨髓细胞反应。不同的机制在起作用,例如细胞凋亡、内毒素耐受性、代谢失败、表观遗传重编程和中枢调节。这会对循环免疫细胞产生全身作用,并影响淋巴器官中的局部祖细胞。在骨髓中,以成熟的中性粒细胞为代价,向着释放未成熟的髓细胞(包括髓源性抑制细胞)的方向逐渐转变。循环树突状细胞数量仍然非常低,单核细胞/巨噬细胞显示出抗炎表型和降低的抗原呈递能力。这些改变的强度和持续性与患者出现有害结果的风险增加有关。因此,骨髓细胞功能障碍在脓毒症获得性免疫缺陷的发生中起重要作用。对于大多数免疫抑制患者,这为评估免疫佐剂分子(粒细胞-巨噬细胞集落刺激因子和干扰素 γ)的临床试验铺平了道路,旨在恢复稳态骨髓细胞反应。我们的综述总结了脓毒症诱导的骨髓细胞功能障碍,以及针对患者这些缺陷提出的当前治疗策略。这些改变的强度和持续性与患者出现有害结果的风险增加有关。因此,骨髓细胞功能障碍在脓毒症获得性免疫缺陷的发生中起重要作用。对于大多数免疫抑制患者,这为评估免疫佐剂分子(粒细胞-巨噬细胞集落刺激因子和干扰素 γ)的临床试验铺平了道路,旨在恢复稳态骨髓细胞反应。我们的综述总结了脓毒症诱导的骨髓细胞功能障碍,以及针对患者这些缺陷提出的当前治疗策略。这些改变的强度和持续性与患者出现有害结果的风险增加有关。因此,骨髓细胞功能障碍在脓毒症获得性免疫缺陷的发生中起重要作用。对于大多数免疫抑制患者,这为评估免疫佐剂分子(粒细胞-巨噬细胞集落刺激因子和干扰素 γ)的临床试验铺平了道路,旨在恢复稳态骨髓细胞反应。我们的综述总结了脓毒症诱导的骨髓细胞功能障碍,以及针对患者这些缺陷提出的当前治疗策略。对于大多数免疫抑制患者,这为评估免疫佐剂分子(粒细胞-巨噬细胞集落刺激因子和干扰素 γ)的临床试验铺平了道路,旨在恢复稳态骨髓细胞反应。我们的综述总结了脓毒症诱导的骨髓细胞功能障碍,以及针对患者这些缺陷提出的当前治疗策略。对于大多数免疫抑制患者,这为评估免疫佐剂分子(粒细胞-巨噬细胞集落刺激因子和干扰素 γ)的临床试验铺平了道路,旨在恢复稳态骨髓细胞反应。我们的综述总结了脓毒症诱导的骨髓细胞功能障碍,以及针对患者这些缺陷提出的当前治疗策略。
更新日期:2020-03-23
中文翻译:

脓毒症获得性免疫缺陷中的髓样细胞
2017 年 5 月,世界卫生组织将败血症确认为全球卫生重点。脓毒症通过引发随时间变化的复杂反应,伴随着促炎和抗炎机制的发生,严重扰乱了免疫稳态。脓毒症严重影响骨髓细胞反应。不同的机制在起作用,例如细胞凋亡、内毒素耐受性、代谢失败、表观遗传重编程和中枢调节。这会对循环免疫细胞产生全身作用,并影响淋巴器官中的局部祖细胞。在骨髓中,以成熟的中性粒细胞为代价,向着释放未成熟的髓细胞(包括髓源性抑制细胞)的方向逐渐转变。循环树突状细胞数量仍然非常低,单核细胞/巨噬细胞显示出抗炎表型和降低的抗原呈递能力。这些改变的强度和持续性与患者出现有害结果的风险增加有关。因此,骨髓细胞功能障碍在脓毒症获得性免疫缺陷的发生中起重要作用。对于大多数免疫抑制患者,这为评估免疫佐剂分子(粒细胞-巨噬细胞集落刺激因子和干扰素 γ)的临床试验铺平了道路,旨在恢复稳态骨髓细胞反应。我们的综述总结了脓毒症诱导的骨髓细胞功能障碍,以及针对患者这些缺陷提出的当前治疗策略。这些改变的强度和持续性与患者出现有害结果的风险增加有关。因此,骨髓细胞功能障碍在脓毒症获得性免疫缺陷的发生中起重要作用。对于大多数免疫抑制患者,这为评估免疫佐剂分子(粒细胞-巨噬细胞集落刺激因子和干扰素 γ)的临床试验铺平了道路,旨在恢复稳态骨髓细胞反应。我们的综述总结了脓毒症诱导的骨髓细胞功能障碍,以及针对患者这些缺陷提出的当前治疗策略。这些改变的强度和持续性与患者出现有害结果的风险增加有关。因此,骨髓细胞功能障碍在脓毒症获得性免疫缺陷的发生中起重要作用。对于大多数免疫抑制患者,这为评估免疫佐剂分子(粒细胞-巨噬细胞集落刺激因子和干扰素 γ)的临床试验铺平了道路,旨在恢复稳态骨髓细胞反应。我们的综述总结了脓毒症诱导的骨髓细胞功能障碍,以及针对患者这些缺陷提出的当前治疗策略。对于大多数免疫抑制患者,这为评估免疫佐剂分子(粒细胞-巨噬细胞集落刺激因子和干扰素 γ)的临床试验铺平了道路,旨在恢复稳态骨髓细胞反应。我们的综述总结了脓毒症诱导的骨髓细胞功能障碍,以及针对患者这些缺陷提出的当前治疗策略。对于大多数免疫抑制患者,这为评估免疫佐剂分子(粒细胞-巨噬细胞集落刺激因子和干扰素 γ)的临床试验铺平了道路,旨在恢复稳态骨髓细胞反应。我们的综述总结了脓毒症诱导的骨髓细胞功能障碍,以及针对患者这些缺陷提出的当前治疗策略。











































 京公网安备 11010802027423号
京公网安备 11010802027423号