JACC: Cardiovascular Interventions ( IF 11.7 ) Pub Date : 2020-04-06 , DOI: 10.1016/j.jcin.2020.01.232 Steven A. Guidera , Sudhir Aggarwal , J. Doyle Walton , David Boland , Roy Jackel , Jeffrey D. Gould , Brooke Kearins , Joseph McGarvey , Yan Qi , Brian Furlong
|
Objectives
The aim of this study was to determine the feasibility of establishing a mechanical thrombectomy (MT) program for acute ischemic stroke in a community hospital using interventional cardiologists working closely with neurologists.
Background
American Heart Association/American Stroke Association 2018 guidelines give a Class I (Level of Evidence: A) recommendation for MT in eligible patients with large vessel occlusion stroke. Improvement in neurological outcomes with MT is highly time sensitive. Most hospitals do not have trained neurointerventionalists to perform MT, leading to treatment delays that reduce the benefit of reperfusion therapy.
Methods
An MT program based in the cardiac catheterization laboratory was developed using interventional cardiologists with ST-segment elevation myocardial infarction teams.
Results
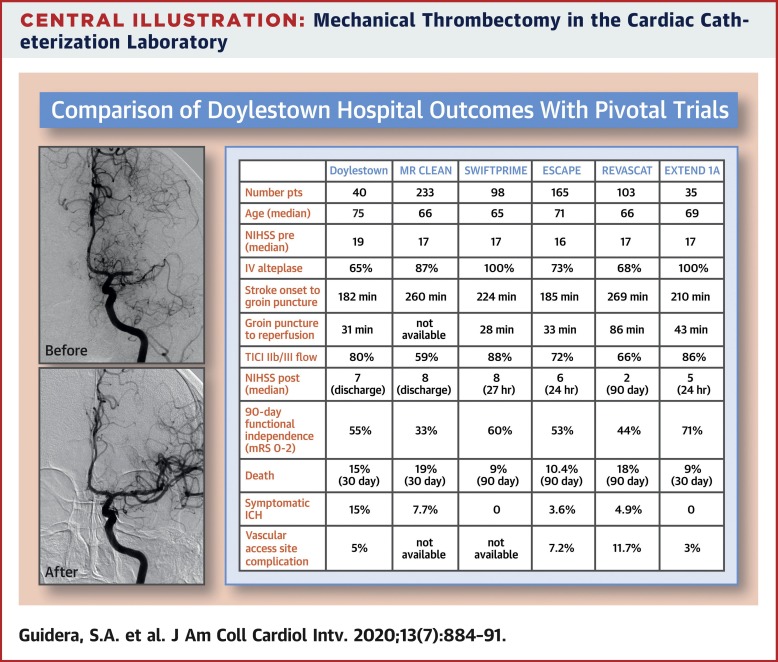
Forty patients underwent attempted MT for acute ischemic stroke. An additional 5 patients who underwent angiography did not undergo attempted thrombectomy, because of absence of target thrombus (n = 4) or unsuitable anatomy (n = 1). Median National Institutes of Health Stroke Scale score prior to MT was 19 and at discharge was 7. TICI (Thrombolysis In Cerebral Infarction) grade 2b or 3 flow was restored in 80% of patients (32 of 40). At 90 days, 55% of patients (22 of 40) were functionally independent (modified Rankin score ≤2). In-hospital mortality was 13% (5 of 40). Symptomatic intracranial hemorrhage occurred in 15% of patients (6 of 40). Major vascular complications occurred in 5% of patients (2 of 40).
Conclusions
MT can be successfully performed by interventional cardiologists with carotid stenting experience working closely with neurologists in hospitals lacking formally trained neurointerventionists. This model has the potential to increase access to timely care for patients with acute ischemic stroke.
中文翻译:

心脏导管实验室中的机械血栓切除术治疗急性缺血性中风
目标
这项研究的目的是确定使用与心脏病专家密切合作的介入心脏病学家在社区医院建立急性缺血性卒中的机械血栓切除术(MT)计划的可行性。
背景
美国心脏协会/美国中风协会2018年指南为符合条件的大血管闭塞性中风患者提供了I级(证据水平:A)建议。MT改善神经系统结果对时间高度敏感。大多数医院没有训练有素的神经介入医师进行MT,导致治疗延误,降低了再灌注治疗的益处。
方法
使用介入式心脏病专家和ST段抬高型心肌梗死团队开发了基于心脏导管实验室的MT程序。
结果
40例接受MT治疗的急性缺血性中风患者。由于没有靶血栓(n = 4)或解剖结构不正确(n = 1),另外5名接受血管造影的患者未进行血栓切除术。美国国立卫生研究院卒中量表评分在MT前为19,出院时为7。TICI(脑梗死溶栓)2b或3级血流在80%的患者中恢复(40分之32)。在90天时,有55%的患者(40名患者中的22名)是功能独立的(改良的Rankin评分≤2)。住院死亡率为13%(40人中有5人)。15%的患者出现症状性颅内出血(40人中有6人)。5%的患者发生了严重的血管并发症(40人中有2人)。
结论
MT可以由具有颈动脉支架置入经验的介入心脏病学家与缺乏正式训练的神经干预专家的医院的神经科医生密切合作来成功完成。该模型有可能增加急性缺血性中风患者及时获得护理的机会。











































 京公网安备 11010802027423号
京公网安备 11010802027423号