当前位置:
X-MOL 学术
›
Modern Pathol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
p53 Immunohistochemical patterns in HPV-related neoplasms of the female lower genital tract can be mistaken for TP53 null or missense mutational patterns.
Modern Pathology ( IF 7.1 ) Pub Date : 2020-04-01 , DOI: 10.1038/s41379-020-0527-y Emily F Thompson 1, 2 , Julia Chen 3 , Jutta Huvila 2 , Jennifer Pors 1, 4 , Hezhen Ren 1, 4 , Julie Ho 3 , Christine Chow 5 , Monica Ta 5 , Lily Proctor 6 , Jessica N McAlpine 6 , David Huntsman 1, 3, 5, 6 , C Blake Gilks 1, 4, 5 , Lynn Hoang 1, 4, 5
Modern Pathology ( IF 7.1 ) Pub Date : 2020-04-01 , DOI: 10.1038/s41379-020-0527-y Emily F Thompson 1, 2 , Julia Chen 3 , Jutta Huvila 2 , Jennifer Pors 1, 4 , Hezhen Ren 1, 4 , Julie Ho 3 , Christine Chow 5 , Monica Ta 5 , Lily Proctor 6 , Jessica N McAlpine 6 , David Huntsman 1, 3, 5, 6 , C Blake Gilks 1, 4, 5 , Lynn Hoang 1, 4, 5
Affiliation
|
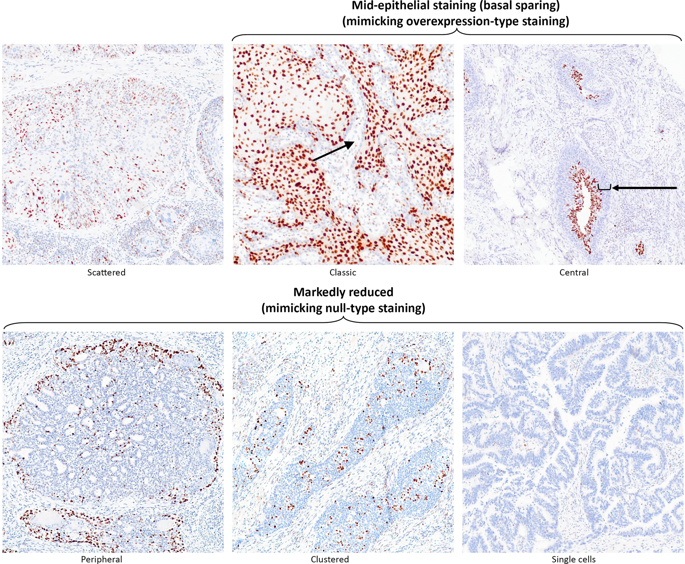
We have recently encountered p53 immunohistochemical (IHC) patterns in human papillomavirus (HPV)-associated carcinomas of the gynecologic tract, which were confused with absent (null) or overexpression TP53 mutational staining. We therefore evaluated p53 and p16 IHC in 25 squamous cell carcinomas (SCC) (16 vulva, 4 Bartholin's gland, and 5 cervix), 20 endocervical adenocarcinomas (EDAC), 14 high-grade squamous intraepithelial lesions (HSIL), 2 adenocarcinoma in situ (AIS), all of which exhibited morphologic features of HPV. Only cases showing diffuse/strong block-like p16 staining were included for further study. All EDACs underwent TP53 sequencing and HPV in situ hybridization (ISH) was performed in selected cases. p53 IHC staining fell into two main patterns. The most common was designated as "markedly reduced (null-like)" (absence or significantly attenuated staining in >70% of cells), which could be confused with true null mutational pattern. This was present in 14/25 (56%) SCCs, 7/14 (50%) HSILs, and 18/20 (90%) EDACs. The second notable pattern was "mid-epithelial (basal sparing)" (distinct absence of staining in basal cells juxtaposed with strong staining in parabasal cells), seen in 10/25 (40%) SCC, 7/14 (50%) HSIL, and none of the EDACs. There was scattered weak to moderate p53 staining (conventional wild type) in 1/25 (4%) SCC and 2/20 (10%) EDAC. No cases showed strong/diffuse overexpression. One EDAC had a TP53 missense mutation and exhibited "markedly reduced (null-like)" staining. HPV ISH revealed an inverse relationship with p53, cells positive for HPV mRNA were negative for p53. Knowledge of these patterns can help pathologists avoid misinterpreting p53 status in the setting of HPVA cancers.
中文翻译:

女性下生殖道 HPV 相关肿瘤中的 p53 免疫组织化学模式可能被误认为是 TP53 无效或错义突变模式。
我们最近遇到了人乳头瘤病毒 (HPV) 相关妇科癌的 p53 免疫组织化学 (IHC) 模式,这些模式与 TP53 突变染色缺失(无效)或过表达相混淆。因此,我们在 25 例鳞状细胞癌 (SCC)(16 例外阴、4 例前庭大腺和 5 例宫颈)、20 例宫颈内膜腺癌 (EDAC)、14 例高级别鳞状上皮内病变 (HSIL)、2 例原位腺癌中评估了 p53 和 p16 IHC (AIS),所有这些都表现出 HPV 的形态学特征。仅包括显示弥漫性/强块状 p16 染色的病例用于进一步研究。所有 EDAC 都进行了 TP53 测序,并在选定的病例中进行了 HPV 原位杂交 (ISH)。p53 IHC 染色分为两种主要模式。最常见的被指定为“显着减少(空样)” (>70% 的细胞中没有染色或染色明显减弱),这可能与真正的无效突变模式相混淆。这存在于 14/25 (56%) SCC、7/14 (50%) HSIL 和 18/20 (90%) EDAC 中。第二个值得注意的模式是“中上皮(基底保留)”(基底细胞明显没有染色,副基底细胞有强染色),见于 10/25 (40%) SCC、7/14 (50%) HSIL ,并且没有任何 EDAC。在 1/25 (4%) SCC 和 2/20 (10%) EDAC 中存在分散的弱至中度 p53 染色(常规野生型)。没有病例表现出强烈/弥漫性过度表达。一个 EDAC 有 TP53 错义突变,并表现出“显着减少(类似无效)”的染色。HPV ISH 显示与 p53 呈反比关系,HPV mRNA 阳性的细胞对 p53 呈阴性。
更新日期:2020-04-24
中文翻译:

女性下生殖道 HPV 相关肿瘤中的 p53 免疫组织化学模式可能被误认为是 TP53 无效或错义突变模式。
我们最近遇到了人乳头瘤病毒 (HPV) 相关妇科癌的 p53 免疫组织化学 (IHC) 模式,这些模式与 TP53 突变染色缺失(无效)或过表达相混淆。因此,我们在 25 例鳞状细胞癌 (SCC)(16 例外阴、4 例前庭大腺和 5 例宫颈)、20 例宫颈内膜腺癌 (EDAC)、14 例高级别鳞状上皮内病变 (HSIL)、2 例原位腺癌中评估了 p53 和 p16 IHC (AIS),所有这些都表现出 HPV 的形态学特征。仅包括显示弥漫性/强块状 p16 染色的病例用于进一步研究。所有 EDAC 都进行了 TP53 测序,并在选定的病例中进行了 HPV 原位杂交 (ISH)。p53 IHC 染色分为两种主要模式。最常见的被指定为“显着减少(空样)” (>70% 的细胞中没有染色或染色明显减弱),这可能与真正的无效突变模式相混淆。这存在于 14/25 (56%) SCC、7/14 (50%) HSIL 和 18/20 (90%) EDAC 中。第二个值得注意的模式是“中上皮(基底保留)”(基底细胞明显没有染色,副基底细胞有强染色),见于 10/25 (40%) SCC、7/14 (50%) HSIL ,并且没有任何 EDAC。在 1/25 (4%) SCC 和 2/20 (10%) EDAC 中存在分散的弱至中度 p53 染色(常规野生型)。没有病例表现出强烈/弥漫性过度表达。一个 EDAC 有 TP53 错义突变,并表现出“显着减少(类似无效)”的染色。HPV ISH 显示与 p53 呈反比关系,HPV mRNA 阳性的细胞对 p53 呈阴性。











































 京公网安备 11010802027423号
京公网安备 11010802027423号