British Journal of Cancer ( IF 6.4 ) Pub Date : 2020-04-03 , DOI: 10.1038/s41416-020-0790-1 Dana Hashim 1 , Birgit Engesæter 1 , Gry Baadstrand Skare 1 , Philip E Castle 2 , Tone Bjørge 1, 3 , Ameli Tropé 1 , Mari Nygård 4
|
Background
HPV16/18 detection may improve cervical cancer risk stratification and better guide which HPV-positive women warrant immediate colposcopy/biopsy. We estimated risks of cervical precancer and cancer by HPV genotype and cytology during the implementation phase of primary HPV testing in Norway.
Methods
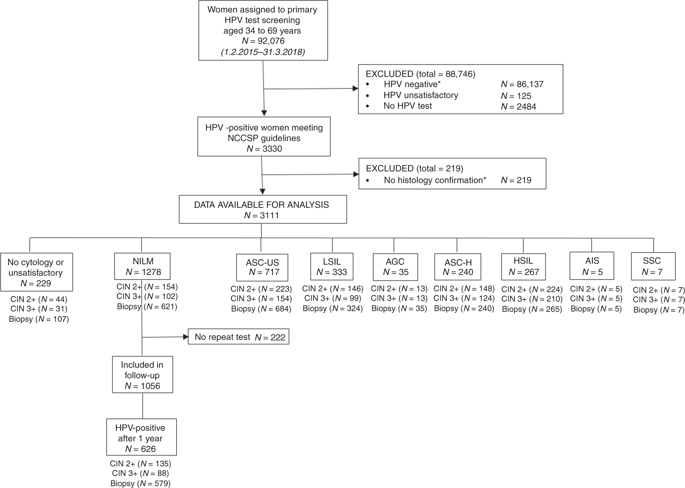
A total of 3111 women, aged 34–69 years, testing HPV-positive at baseline and undergoing cytology testing from February 2015 to April 2018 had data available for analysis. Risk estimates with 95% confidence intervals (95%CIs) of cervical intraepithelial neoplasia grade 3 or more severe (CIN3+) were estimated for cytology results and HPV genotypes (HPV16, HPV18, and other high-risk HPV).
Results
CIN3+ risks were higher for HPV16/18 than other high-risk HPV genotypes. Among women with any cytologic abnormality [atypical squamous cells of undetermined significance or worse], immediate risks were 57.8% (95%CI = 53.0–62.6%) for HPV16, 40.2% (95%CI = 32.3–49.2%) for HPV18, and 31.4% (95%CI = 28.7–34.3%) for other high-risk HPV. Among those with normal cytology, CIN3+ risks were 19.9% (95%CI = 15.0–26.1%) for HPV16 positives, 10.8% (95%CI = 5.6–20.5%) for HPV18 positives, and 5.5% (95%CI = 4.2–7.1%) for other high-risk HPV.
Conclusions
The benefits and harms of managing women based on HPV positivity and cytology results can be better balanced by inclusion of HPV genotyping in screening and choosing more conservative management for other high-risk HPV compared to HPV16/18.
中文翻译:

通过细胞学和 HPV 基因型对宫颈癌风险进行分层的真实世界数据可为常规宫颈筛查中 HPV 阳性女性的管理提供信息。
背景
HPV16/18 检测可以改善宫颈癌风险分层,并更好地指导哪些 HPV 阳性女性需要立即进行阴道镜检查/活检。我们在挪威初级 HPV 检测的实施阶段通过 HPV 基因型和细胞学评估了宫颈癌前病变和癌症的风险。
方法
在 2015 年 2 月至 2018 年 4 月期间,共有 3111 名年龄在 34-69 岁之间的基线 HPV 检测呈阳性并接受细胞学检测的女性获得了可用于分析的数据。细胞学结果和 HPV 基因型(HPV16、HPV18 和其他高危 HPV)的宫颈上皮内瘤变 3 级或更严重 (CIN3+) 的风险估计具有 95% 置信区间 (95%CI)。
结果
HPV16/18 的 CIN3+ 风险高于其他高风险 HPV 基因型。在有任何细胞学异常 [意义未明或更严重的非典型鳞状细胞] 的女性中,HPV16 的直接风险为 57.8% (95%CI = 53.0–62.6%),HPV18 的直接风险为 40.2% (95%CI = 32.3–49.2%),其他高危 HPV 为 31.4% (95%CI = 28.7–34.3%)。在细胞学正常的人群中,HPV16 阳性的 CIN3+ 风险为 19.9% (95%CI = 15.0–26.1%),HPV18 阳性的风险为 10.8% (95%CI = 5.6–20.5%),HPV18 阳性的风险为 5.5% (95%CI = 4.2) –7.1%) 对于其他高危 HPV。
结论
与 HPV16/18 相比,通过将 HPV 基因分型纳入筛查并为其他高危 HPV 选择更保守的管理,可以更好地平衡根据 HPV 阳性和细胞学结果管理女性的利弊。










































 京公网安备 11010802027423号
京公网安备 11010802027423号