Prostate Cancer and Prostatic Diseases ( IF 5.1 ) Pub Date : 2020-03-30 , DOI: 10.1038/s41391-020-0226-2 Jeffrey J Tosoian 1 , Samuel R Birer 2 , R Jeffrey Karnes 3 , Jingbin Zhang 4 , Elai Davicioni 4 , Eric E Klein 5 , Stephen J Freedland 6 , Sheila Weinmann 7 , Bruce J Trock 8 , Robert T Dess 2 , Shuang G Zhao 2 , William C Jackson 2 , Kosj Yamoah 9 , Alan Dal Pra 10 , Brandon A Mahal 11 , Todd M Morgan 1 , Rohit Mehra 12 , Samuel Kaffenberger 1 , Simpa S Salami 1 , Christopher Kane 13 , Alan Pollack 10 , Robert B Den 14 , Alejandro Berlin 15 , Edward M Schaeffer 16 , Paul L Nguyen 11 , Felix Y Feng 17 , Daniel E Spratt 2
|
Background
Prostate cancer exhibits biological and clinical heterogeneity even within established clinico-pathologic risk groups. The Decipher genomic classifier (GC) is a validated method to further risk-stratify disease in patients with prostate cancer, but its performance solely within National Comprehensive Cancer Network (NCCN) high-risk disease has not been undertaken to date.
Methods
A multi-institutional retrospective study of 405 men with high-risk prostate cancer who underwent primary treatment with radical prostatectomy (RP) or radiation therapy (RT) with androgen-deprivation therapy (ADT) at 11 centers from 1995 to 2005 was performed. Cox proportional hazards models were used to determine the hazard ratios (HR) for the development of metastatic disease based on clinico-pathologic variables, risk groups, and GC score. The area under the receiver operating characteristic curve (AUC) was determined for regression models without and with the GC score.
Results
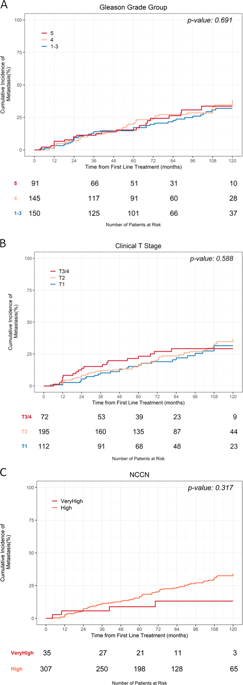
Over a median follow-up of 82 months, 104 patients (26%) developed metastatic disease. On univariable analysis, increasing GC score was significantly associated with metastatic disease ([HR]: 1.34 per 0.1 unit increase, 95% confidence interval [CI]: 1.19–1.50, p < 0.001), while age, serum PSA, biopsy GG, and clinical T-stage were not (all p > 0.05). On multivariable analysis, GC score (HR: 1.33 per 0.1 unit increase, 95% CI: 1.19–1.48, p < 0.001) and GC high-risk (vs low-risk, HR: 2.95, 95% CI: 1.79–4.87, p < 0.001) were significantly associated with metastasis. The addition of GC score to regression models based on NCCN risk group improved model AUC from 0.46 to 0.67, and CAPRA from 0.59 to 0.71.
Conclusions
Among men with high-risk prostate cancer, conventional clinico-pathologic data had poor discrimination to risk stratify development of metastatic disease. GC score was a significant and independent predictor of metastasis and may help identify men best suited for treatment intensification/de-escalation.
中文翻译:

高危局限性前列腺癌男性临床病理模型的表现:22 基因基因组分类器的影响
背景
即使在既定的临床病理风险组中,前列腺癌也表现出生物学和临床异质性。Decipher 基因组分类器 (GC) 是一种经过验证的方法,可进一步对前列腺癌患者的疾病进行风险分层,但迄今为止尚未仅在国家综合癌症网络 (NCCN) 高危疾病中发挥其作用。
方法
对 1995 年至 2005 年在 11 个中心接受根治性前列腺切除术 (RP) 或放射治疗 (RT) 和雄激素剥夺疗法 (ADT) 的主要治疗的 405 名高危前列腺癌男性进行了多机构回顾性研究。Cox 比例风险模型用于根据临床病理变量、风险组和 GC 评分确定转移性疾病发展的风险比 (HR)。对于没有和有 GC 评分的回归模型,确定了接受者操作特征曲线 (AUC) 下的面积。
结果
在 82 个月的中位随访期间,104 名患者 (26%) 发生了转移性疾病。在单变量分析中,GC 评分增加与转移性疾病显着相关([HR]:每 0.1 个单位增加 1.34,95% 置信区间 [CI]:1.19–1.50,p < 0.001),而年龄、血清 PSA、活检GG 、和临床 T 阶段没有(所有p > 0.05)。在多变量分析中,GC 评分(HR:1.33 每增加 0.1 个单位,95% CI:1.19–1.48,p < 0.001)和 GC 高风险(与低风险相比,HR:2.95,95% CI:1.79–4.87,p < 0.001) 与转移显着相关。将 GC 分数添加到基于 NCCN 风险组的回归模型中,将模型 AUC 从 0.46 提高到 0.67,将 CAPRA 从 0.59 提高到 0.71。
结论
在患有高危前列腺癌的男性中,传统的临床病理学数据难以区分转移性疾病的风险分层。GC 评分是转移的重要且独立的预测因子,可能有助于确定最适合治疗强化/降级的男性。











































 京公网安备 11010802027423号
京公网安备 11010802027423号