当前位置:
X-MOL 学术
›
JAMA Intern. Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Association of the Comprehensive End-Stage Renal Disease Care Model With Medicare Payments and Quality of Care for Beneficiaries With End-Stage Renal Disease
JAMA Internal Medicine ( IF 22.5 ) Pub Date : 2020-06-01 , DOI: 10.1001/jamainternmed.2020.0562 Grecia Marrufo 1 , Erin Murphy Colligan 2 , Brighita Negrusa 1 , Darin Ullman 1 , Joe Messana 3 , Anand Shah 4 , Tom Duvall 4 , Richard A Hirth 4
JAMA Internal Medicine ( IF 22.5 ) Pub Date : 2020-06-01 , DOI: 10.1001/jamainternmed.2020.0562 Grecia Marrufo 1 , Erin Murphy Colligan 2 , Brighita Negrusa 1 , Darin Ullman 1 , Joe Messana 3 , Anand Shah 4 , Tom Duvall 4 , Richard A Hirth 4
Affiliation
|
Importance
Medicare beneficiaries with end-stage renal disease (ESRD) are a medically complex group accounting for less than 1% of the Medicare population but more than 7% of Medicare fee-for-service payments. Objective
To evaluate the association of the Comprehensive End-Stage Renal Disease Care (CEC) model with Medicare payments, health care use, and quality of care. Design, Setting, and Participants
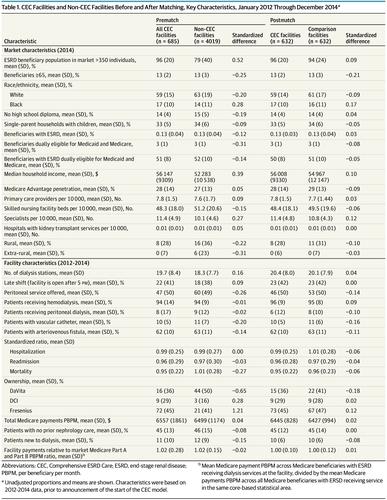
In this economic evaluation, a difference-in-differences design estimated the change in outcomes for 73 094 Medicare fee-for-service beneficiaries aligned to CEC dialysis facilities between the baseline (from January 2014 to March 2015) and intervention periods (from October 2015 to December 2017) relative to 60 464 beneficiaries at matched dialysis facilities. In the CEC model, dialysis facilities, nephrologists, and other providers partner to form ESRD Seamless Care Organizations (ESCOs), specialty-oriented accountable care organizations that coordinate care for beneficiaries with ESRD. ESCOs with expenditures below a benchmark set by the Centers for Medicare & Medicaid Services are eligible to share in savings if they meet quality thresholds. A total of 685 dialysis facilities affiliated with 37 ESCOs participated in the CEC model as of January 2017. Thirteen ESCOs joined the CEC model on October 1, 2015 (wave 1), and 24 ESCOs joined on January 1, 2017 (wave 2). Patients with ESRD who were aligned with CEC dialysis facilities were compared with patients at matched dialysis facilities. Main Outcomes and Measures
Medicare total and service-specific payments per beneficiary per month; hospitalizations, readmissions, and emergency department visits; and select quality measures. Results
Relative to the comparison group (n = 60 464; 55% men; mean [SD] age, 63.5 [14.4] years), total Medicare payments for CEC beneficiaries (n = 73 094; 56% men; mean [SD] age, 63.0 [14.4] years) decreased by $114 in payments per beneficiary per month (95% CI, -$202 to -$26; P = .01), associated primarily with decreases in payments for hospitalizations and readmissions. Payment reductions were offset by shared savings payments to ESCOs, resulting in net losses of $78 in payments per beneficiary per month (95% CI, -$8 to $164; P = .07). Relative to the comparison group, CEC beneficiaries had 5.01 fewer hospitalizations per 1000 beneficiaries per month (95% CI, -8.45 to -1.56; P = .004), as well as fewer catheter placements (CEC beneficiaries with catheter as vascular access for periods longer than 90 days decreased by 0.78 percentage points [95% CI, -1.36 to -0.19; P = .01]) and fewer hospitalizations for ESRD complications (CEC beneficiaries were 0.11 percentage points less likely [95% CI, -0.20 to -0.02; P = .01] to be hospitalized in a given month). Total dialysis sessions and payments increased, suggesting improved adherence to dialysis treatments. Conclusions and Relevance
Early findings from the CEC model demonstrate that a specialty accountable care organization model focused on a particular population was associated with reduced payments and improved quality of care. Future research can assess the longer-term outcomes of the CEC model and its applicability to populations with other complex chronic conditions.
中文翻译:

终末期肾病综合护理模式与终末期肾病受益人的医疗保险支付和护理质量的关联
重要性 患有终末期肾病 (ESRD) 的医疗保险受益人是一个医学复杂的群体,占医疗保险人口的不到 1%,但占医疗保险按服务付费的 7% 以上。目的评估综合终末期肾病护理 (CEC) 模型与医疗保险支付、医疗保健使用和护理质量的关联。设计、设置和参与者 在此经济评估中,差异设计估计了与 CEC 透析设施一致的 73 094 名医疗保险按服务收费受益人在基线(2014 年 1 月至 2015 年 3 月)和干预期间(从 2015 年 10 月到 2017 年 12 月)相对于匹配透析设施的 60 464 名受益人。在 CEC 模型中,透析设施、肾病学家、和其他提供者合作组建 ESRD 无缝护理组织 (ESCO),这是一种以专业为导向的负责任的护理组织,负责协调对受益人的护理与 ESRD。支出低于医疗保险和医疗补助服务中心设定的基准的 ESCO,如果达到质量阈值,则有资格分享储蓄。截至 2017 年 1 月,共有 37 家 ESCO 下属的 685 家透析设施参与了 CEC 模型。 13 家 ESCO 于 2015 年 10 月 1 日(第一波)加入了 CEC 模型,24 家 ESCO 于 2017 年 1 月 1 日(第二波)加入。将使用 CEC 透析设施的 ESRD 患者与匹配的透析设施中的患者进行比较。主要结果和措施 每个受益人每月的医疗保险总额和特定服务付款;住院、再入院和急诊就诊;并选择质量措施。结果 相对于对照组(n = 60 464;55% 男性;平均 [SD] 年龄,63.5 [14.4] 岁),CEC 受益人的医疗保险支付总额(n = 73 094;56% 男性;平均 [SD] 年龄) , 63.0 [14.4] 年)每个受益人每月的付款减少了 114 美元(95% CI,-$202 至 -$26;P = .01),主要与住院和再入院付款的减少有关。减少的付款被对 ESCO 的共享储蓄付款所抵消,导致每个受益人每月的付款净损失为 78 美元(95% CI,-8 美元至 164 美元;P = .07)。相对于对照组,CEC 受益人每月每 1000 名受益人的住院次数减少 5.01(95% CI,-8.45 至 -1.56;P = .004),以及更少的导管放置(使用导管作为血管通路超过 90 天的 CEC 受益人减少了 0.78 个百分点 [95% CI,-1.36 至 -0.19;P = .01])和更少的 ESRD 并发症住院治疗(CEC受益人在给定月份住院的可能性降低了 0.11 个百分点 [95% CI,-0.20 至 -0.02;P = .01])。总透析次数和付款增加,表明对透析治疗的依从性提高。结论和相关性 CEC 模型的早期发现表明,专注于特定人群的专业责任护理组织模型与减少付款和提高护理质量有关。未来的研究可以评估 CEC 模型的长期结果及其对其他复杂慢性病人群的适用性。78 个百分点 [95% CI,-1.36 至 -0.19;P = .01])和更少因 ESRD 并发症住院(CEC 受益人在给定月份住院的可能性降低 0.11 个百分点 [95% CI,-0.20 至 -0.02;P = .01])。总透析次数和付款增加,表明对透析治疗的依从性提高。结论和相关性 CEC 模型的早期发现表明,专注于特定人群的专业责任护理组织模型与减少付款和提高护理质量有关。未来的研究可以评估 CEC 模型的长期结果及其对其他复杂慢性病人群的适用性。78 个百分点 [95% CI,-1.36 至 -0.19;P = .01])和更少因 ESRD 并发症住院(CEC 受益人在给定月份住院的可能性降低 0.11 个百分点 [95% CI,-0.20 至 -0.02;P = .01])。总透析次数和付款增加,表明对透析治疗的依从性提高。结论和相关性 CEC 模型的早期发现表明,专注于特定人群的专业责任护理组织模型与减少付款和提高护理质量有关。未来的研究可以评估 CEC 模型的长期结果及其对其他复杂慢性病人群的适用性。可能性降低 11 个百分点 [95% CI,-0.20 至 -0.02;P = .01] 在给定月份住院)。总透析次数和付款增加,表明对透析治疗的依从性提高。结论和相关性 CEC 模型的早期发现表明,专注于特定人群的专业责任护理组织模型与减少付款和提高护理质量有关。未来的研究可以评估 CEC 模型的长期结果及其对其他复杂慢性病人群的适用性。可能性降低 11 个百分点 [95% CI,-0.20 至 -0.02;P = .01] 在给定月份住院)。总透析次数和付款增加,表明对透析治疗的依从性提高。结论和相关性 CEC 模型的早期发现表明,专注于特定人群的专业责任护理组织模型与减少付款和提高护理质量有关。未来的研究可以评估 CEC 模型的长期结果及其对其他复杂慢性病人群的适用性。结论和相关性 CEC 模型的早期发现表明,专注于特定人群的专业责任护理组织模型与减少付款和提高护理质量有关。未来的研究可以评估 CEC 模型的长期结果及其对其他复杂慢性病人群的适用性。结论和相关性 CEC 模型的早期发现表明,专注于特定人群的专业责任护理组织模型与减少付款和提高护理质量有关。未来的研究可以评估 CEC 模型的长期结果及其对其他复杂慢性病人群的适用性。
更新日期:2020-06-01
中文翻译:

终末期肾病综合护理模式与终末期肾病受益人的医疗保险支付和护理质量的关联
重要性 患有终末期肾病 (ESRD) 的医疗保险受益人是一个医学复杂的群体,占医疗保险人口的不到 1%,但占医疗保险按服务付费的 7% 以上。目的评估综合终末期肾病护理 (CEC) 模型与医疗保险支付、医疗保健使用和护理质量的关联。设计、设置和参与者 在此经济评估中,差异设计估计了与 CEC 透析设施一致的 73 094 名医疗保险按服务收费受益人在基线(2014 年 1 月至 2015 年 3 月)和干预期间(从 2015 年 10 月到 2017 年 12 月)相对于匹配透析设施的 60 464 名受益人。在 CEC 模型中,透析设施、肾病学家、和其他提供者合作组建 ESRD 无缝护理组织 (ESCO),这是一种以专业为导向的负责任的护理组织,负责协调对受益人的护理与 ESRD。支出低于医疗保险和医疗补助服务中心设定的基准的 ESCO,如果达到质量阈值,则有资格分享储蓄。截至 2017 年 1 月,共有 37 家 ESCO 下属的 685 家透析设施参与了 CEC 模型。 13 家 ESCO 于 2015 年 10 月 1 日(第一波)加入了 CEC 模型,24 家 ESCO 于 2017 年 1 月 1 日(第二波)加入。将使用 CEC 透析设施的 ESRD 患者与匹配的透析设施中的患者进行比较。主要结果和措施 每个受益人每月的医疗保险总额和特定服务付款;住院、再入院和急诊就诊;并选择质量措施。结果 相对于对照组(n = 60 464;55% 男性;平均 [SD] 年龄,63.5 [14.4] 岁),CEC 受益人的医疗保险支付总额(n = 73 094;56% 男性;平均 [SD] 年龄) , 63.0 [14.4] 年)每个受益人每月的付款减少了 114 美元(95% CI,-$202 至 -$26;P = .01),主要与住院和再入院付款的减少有关。减少的付款被对 ESCO 的共享储蓄付款所抵消,导致每个受益人每月的付款净损失为 78 美元(95% CI,-8 美元至 164 美元;P = .07)。相对于对照组,CEC 受益人每月每 1000 名受益人的住院次数减少 5.01(95% CI,-8.45 至 -1.56;P = .004),以及更少的导管放置(使用导管作为血管通路超过 90 天的 CEC 受益人减少了 0.78 个百分点 [95% CI,-1.36 至 -0.19;P = .01])和更少的 ESRD 并发症住院治疗(CEC受益人在给定月份住院的可能性降低了 0.11 个百分点 [95% CI,-0.20 至 -0.02;P = .01])。总透析次数和付款增加,表明对透析治疗的依从性提高。结论和相关性 CEC 模型的早期发现表明,专注于特定人群的专业责任护理组织模型与减少付款和提高护理质量有关。未来的研究可以评估 CEC 模型的长期结果及其对其他复杂慢性病人群的适用性。78 个百分点 [95% CI,-1.36 至 -0.19;P = .01])和更少因 ESRD 并发症住院(CEC 受益人在给定月份住院的可能性降低 0.11 个百分点 [95% CI,-0.20 至 -0.02;P = .01])。总透析次数和付款增加,表明对透析治疗的依从性提高。结论和相关性 CEC 模型的早期发现表明,专注于特定人群的专业责任护理组织模型与减少付款和提高护理质量有关。未来的研究可以评估 CEC 模型的长期结果及其对其他复杂慢性病人群的适用性。78 个百分点 [95% CI,-1.36 至 -0.19;P = .01])和更少因 ESRD 并发症住院(CEC 受益人在给定月份住院的可能性降低 0.11 个百分点 [95% CI,-0.20 至 -0.02;P = .01])。总透析次数和付款增加,表明对透析治疗的依从性提高。结论和相关性 CEC 模型的早期发现表明,专注于特定人群的专业责任护理组织模型与减少付款和提高护理质量有关。未来的研究可以评估 CEC 模型的长期结果及其对其他复杂慢性病人群的适用性。可能性降低 11 个百分点 [95% CI,-0.20 至 -0.02;P = .01] 在给定月份住院)。总透析次数和付款增加,表明对透析治疗的依从性提高。结论和相关性 CEC 模型的早期发现表明,专注于特定人群的专业责任护理组织模型与减少付款和提高护理质量有关。未来的研究可以评估 CEC 模型的长期结果及其对其他复杂慢性病人群的适用性。可能性降低 11 个百分点 [95% CI,-0.20 至 -0.02;P = .01] 在给定月份住院)。总透析次数和付款增加,表明对透析治疗的依从性提高。结论和相关性 CEC 模型的早期发现表明,专注于特定人群的专业责任护理组织模型与减少付款和提高护理质量有关。未来的研究可以评估 CEC 模型的长期结果及其对其他复杂慢性病人群的适用性。结论和相关性 CEC 模型的早期发现表明,专注于特定人群的专业责任护理组织模型与减少付款和提高护理质量有关。未来的研究可以评估 CEC 模型的长期结果及其对其他复杂慢性病人群的适用性。结论和相关性 CEC 模型的早期发现表明,专注于特定人群的专业责任护理组织模型与减少付款和提高护理质量有关。未来的研究可以评估 CEC 模型的长期结果及其对其他复杂慢性病人群的适用性。











































 京公网安备 11010802027423号
京公网安备 11010802027423号