当前位置:
X-MOL 学术
›
J. Am. Coll. Cardiol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Ticagrelor with or without Aspirin in High-Risk Patients with Diabetes Mellitus undergoing Percutaneous Coronary Intervention
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2020-05-01 , DOI: 10.1016/j.jacc.2020.03.008 Dominick J Angiolillo 1 , Usman Baber 2 , Samantha Sartori 2 , Carlo Briguori 3 , George Dangas 2 , David J Cohen 4 , Shamir R Mehta 5 , C Michael Gibson 6 , Rishi Chandiramani 2 , Kurt Huber 7 , Ran Kornowski 8 , Giora Weisz 9 , Vijay Kunadian 10 , Keith G Oldroyd 11 , Han Ya-Ling 12 , Upendra Kaul 13 , Bernhard Witzenbichler 14 , Dariusz Dudek 15 , Gennaro Sardella 16 , Javier Escaned 17 , Samin Sharma 2 , Richard A Shlofmitz 18 , Timothy Collier 19 , Stuart Pocock 19 , Roxana Mehran 2
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2020-05-01 , DOI: 10.1016/j.jacc.2020.03.008 Dominick J Angiolillo 1 , Usman Baber 2 , Samantha Sartori 2 , Carlo Briguori 3 , George Dangas 2 , David J Cohen 4 , Shamir R Mehta 5 , C Michael Gibson 6 , Rishi Chandiramani 2 , Kurt Huber 7 , Ran Kornowski 8 , Giora Weisz 9 , Vijay Kunadian 10 , Keith G Oldroyd 11 , Han Ya-Ling 12 , Upendra Kaul 13 , Bernhard Witzenbichler 14 , Dariusz Dudek 15 , Gennaro Sardella 16 , Javier Escaned 17 , Samin Sharma 2 , Richard A Shlofmitz 18 , Timothy Collier 19 , Stuart Pocock 19 , Roxana Mehran 2
Affiliation
|
BACKGROUND
P2Y12 inhibitor monotherapy with ticagrelor after a brief period of dual antiplatelet therapy can reduce bleeding without increasing ischemic harm after percutaneous coronary intervention (PCI). The impact of this approach among patients with diabetes mellitus (DM) remains unknown. OBJECTIVES
To examine the effect of ticagrelor monotherapy versus ticagrelor plus aspirin among patients with DM undergoing PCI. METHODS
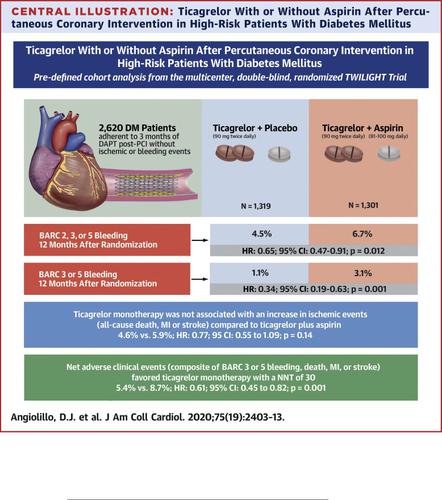
This was a pre-specified analysis of the DM cohort in the TWILIGHT trial. After 3 months of ticagrelor plus aspirin, patients were maintained on ticagrelor and randomized to aspirin or placebo for 1 year. The primary endpoint was Bleeding Academic Research Consortium (BARC) 2, 3 or 5 bleeding. The composite ischemic endpoint was all-cause death, myocardial infarction, or stroke. RESULTS
Patients with DM comprised 37% (n=2620) of the randomized cohort and were characterized by more frequent comorbidities and a higher prevalence of multivessel disease. The incidence of BARC 2, 3 or 5 bleeding was 4.5% and 6.7% among patients with DM randomized to ticagrelor plus placebo versus ticagrelor plus aspirin (HR 0.65; 95% CI 0.47-0.91; p=0.012). Ticagrelor monotherapy was not associated with an increase in ischemic events compared with ticagrelor plus aspirin (4.6% vs 5.9%; HR 0.77; 95% CI 0.55 to 1.09; p=0.14). In the overall trial population, there was no significant interaction between DM status and treatment group for the primary bleeding or ischemic endpoints. CONCLUSIONS
Compared with ticagrelor plus aspirin, the effect of ticagrelor monotherapy in reducing the risk of clinically relevant bleeding without any increase in ischemic events was consistent among patients with or without DM undergoing PCI.
中文翻译:

替格瑞洛联合或不联合阿司匹林治疗接受经皮冠状动脉介入治疗的高危糖尿病患者
背景 在短暂的双重抗血小板治疗后,P2Y12 抑制剂与替格瑞洛单药治疗可以减少出血,而不会增加经皮冠状动脉介入治疗 (PCI) 后的缺血性损害。这种方法对糖尿病 (DM) 患者的影响仍然未知。目的 检验替格瑞洛单药治疗与替格瑞洛加阿司匹林对接受 PCI 的 DM 患者的影响。方法 这是对 TWILIGHT 试验中 DM 队列的预先指定分析。替格瑞洛加阿司匹林 3 个月后,患者继续服用替格瑞洛并随机分配至阿司匹林或安慰剂组 1 年。主要终点是出血学术研究联盟 (BARC) 2、3 或 5 次出血。复合缺血终点是全因死亡、心肌梗塞或中风。结果 DM 患者占随机队列的 37% (n=2620),其特征是合并症更频繁,多支血管疾病患病率更高。在随机分配至替格瑞洛加安慰剂组与替格瑞洛加阿司匹林组的 DM 患者中,BARC 2、3 或 5 次出血的发生率分别为 4.5% 和 6.7%(HR 0.65;95% CI 0.47-0.91;p=0.012)。与替格瑞洛联合阿司匹林相比,替格瑞洛单药治疗与缺血事件增加无关(4.6% vs 5.9%;HR 0.77;95% CI 0.55 至 1.09;p=0.14)。在整个试验人群中,DM 状态与治疗组之间在主要出血或缺血终点方面没有显着的相互作用。结论与替格瑞洛加阿司匹林相比,
更新日期:2020-05-01
中文翻译:

替格瑞洛联合或不联合阿司匹林治疗接受经皮冠状动脉介入治疗的高危糖尿病患者
背景 在短暂的双重抗血小板治疗后,P2Y12 抑制剂与替格瑞洛单药治疗可以减少出血,而不会增加经皮冠状动脉介入治疗 (PCI) 后的缺血性损害。这种方法对糖尿病 (DM) 患者的影响仍然未知。目的 检验替格瑞洛单药治疗与替格瑞洛加阿司匹林对接受 PCI 的 DM 患者的影响。方法 这是对 TWILIGHT 试验中 DM 队列的预先指定分析。替格瑞洛加阿司匹林 3 个月后,患者继续服用替格瑞洛并随机分配至阿司匹林或安慰剂组 1 年。主要终点是出血学术研究联盟 (BARC) 2、3 或 5 次出血。复合缺血终点是全因死亡、心肌梗塞或中风。结果 DM 患者占随机队列的 37% (n=2620),其特征是合并症更频繁,多支血管疾病患病率更高。在随机分配至替格瑞洛加安慰剂组与替格瑞洛加阿司匹林组的 DM 患者中,BARC 2、3 或 5 次出血的发生率分别为 4.5% 和 6.7%(HR 0.65;95% CI 0.47-0.91;p=0.012)。与替格瑞洛联合阿司匹林相比,替格瑞洛单药治疗与缺血事件增加无关(4.6% vs 5.9%;HR 0.77;95% CI 0.55 至 1.09;p=0.14)。在整个试验人群中,DM 状态与治疗组之间在主要出血或缺血终点方面没有显着的相互作用。结论与替格瑞洛加阿司匹林相比,











































 京公网安备 11010802027423号
京公网安备 11010802027423号