当前位置:
X-MOL 学术
›
J. Hepatol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Changes in frailty are associated with waitlist mortality in patients with cirrhosis
Journal of Hepatology ( IF 26.8 ) Pub Date : 2020-09-01 , DOI: 10.1016/j.jhep.2020.03.029 Jennifer C Lai 1 , Jennifer L Dodge 2 , Matthew R Kappus 3 , Michael A Dunn 4 , Michael L Volk 5 , Andres Duarte-Rojo 6 , Daniel R Ganger 7 , Robert S Rahimi 8 , Charles E McCulloch 9 , Christine E Haugen 10 , Mara McAdams-DeMarco 11 , Daniela P Ladner 12 , Dorry L Segev 10 , Elizabeth C Verna 13 ,
Journal of Hepatology ( IF 26.8 ) Pub Date : 2020-09-01 , DOI: 10.1016/j.jhep.2020.03.029 Jennifer C Lai 1 , Jennifer L Dodge 2 , Matthew R Kappus 3 , Michael A Dunn 4 , Michael L Volk 5 , Andres Duarte-Rojo 6 , Daniel R Ganger 7 , Robert S Rahimi 8 , Charles E McCulloch 9 , Christine E Haugen 10 , Mara McAdams-DeMarco 11 , Daniela P Ladner 12 , Dorry L Segev 10 , Elizabeth C Verna 13 ,
Affiliation
|
BACKGROUND & AIMS
Frailty is predictive of death in patients with cirrhosis, but studies to date have been limited to assessments at a single time point. We aimed to evaluate changes in frailty over time (ΔLFI) and its association with death/delisting for sickness. METHODS
Adults with cirrhosis listed for liver transplantation without hepatocellular carcinoma at 8 U.S. centers underwent ambulatory longitudinal frailty testing with the Liver Frailty Index (LFI). We used multilevel linear mixed effects regression to model and predict ΔLFI per 3 months based on age, gender, MELDNa, ascites, and hepatic encephalopathy (HE) and categorize patients by frailty trajectories. Competing risk regression evaluated the subhazard ratio (sHR) of baseline LFI and predicted ΔLFI on death/delisting, with transplantation as the competing risk. RESULTS
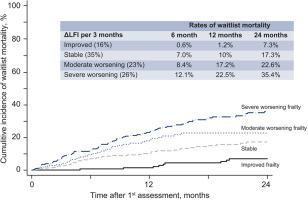
We analyzed 2,851 visits from 1,093 outpatients with cirrhosis. Patients with severe frailty worsening had worse baseline LFI and were more likely to have NAFLD, diabetes, or dialysis-dependence. After a median follow-up of 11 months, 223 (20%) of the overall cohort died/were delisted for sickness. The cumulative incidence of death/delisting increased by worsening ΔLFI group. In competing risk regression adjusted for baseline LFI, age, height, MELDNa, and albumin, a 0.1 unit change in ΔLFI per 3 months was associated with a 2.04-fold increased risk of death/delisting (95% CI, 1.35-3.09). CONCLUSION
Changes in frailty were significantly associated with death/delisting independent of baseline frailty and MELDNa. Notably, patients who experienced improvements in frailty over time had a lower risk of death/delisting than those who experienced worsening frailty. Our data support the longitudinal measurement of frailty, using the LFI, in patients with cirrhosis and lay the foundation for interventional work aimed at reversing frailty.
中文翻译:

虚弱的变化与肝硬化患者的候补死亡率相关
背景和目的 虚弱是肝硬化患者死亡的预测因素,但迄今为止的研究仅限于单个时间点的评估。我们的目的是评估衰弱随时间的变化(ΔLFI)及其与死亡/因病退市的关系。方法 在美国 8 个中心,对未患肝细胞癌的肝硬化成人患者进行肝脏衰弱指数 (LFI) 动态纵向衰弱测试。我们使用多级线性混合效应回归根据年龄、性别、MELDNa、腹水和肝性脑病 (HE) 来建模和预测每 3 个月的 ΔLFI,并按衰弱轨迹对患者进行分类。竞争风险回归评估了基线 LFI 的亚危险比 (sHR),并预测了死亡/退市时的 ΔLFI,其中移植作为竞争风险。结果 我们分析了 1,093 名肝硬化门诊患者的 2,851 次就诊。虚弱严重恶化的患者基线 LFI 较差,并且更有可能患有 NAFLD、糖尿病或透析依赖。中位随访 11 个月后,整个队列中有 223 人 (20%) 死亡/因病被除名。 ΔLFI 组恶化导致死亡/退市的累积发生率增加。在根据基线 LFI、年龄、身高、MELDNa 和白蛋白进行调整的竞争风险回归中,每 3 个月 ΔLFI 变化 0.1 个单位,死亡/退市风险增加 2.04 倍(95% CI,1.35-3.09)。结论 虚弱变化与死亡/退市显着相关,与基线虚弱和 MELDNa 无关。值得注意的是,随着时间的推移,虚弱状况有所改善的患者比虚弱状况恶化的患者死亡/退市的风险更低。 我们的数据支持使用 LFI 对肝硬化患者的衰弱进行纵向测量,并为旨在逆转衰弱的介入工作奠定基础。
更新日期:2020-09-01
中文翻译:

虚弱的变化与肝硬化患者的候补死亡率相关
背景和目的 虚弱是肝硬化患者死亡的预测因素,但迄今为止的研究仅限于单个时间点的评估。我们的目的是评估衰弱随时间的变化(ΔLFI)及其与死亡/因病退市的关系。方法 在美国 8 个中心,对未患肝细胞癌的肝硬化成人患者进行肝脏衰弱指数 (LFI) 动态纵向衰弱测试。我们使用多级线性混合效应回归根据年龄、性别、MELDNa、腹水和肝性脑病 (HE) 来建模和预测每 3 个月的 ΔLFI,并按衰弱轨迹对患者进行分类。竞争风险回归评估了基线 LFI 的亚危险比 (sHR),并预测了死亡/退市时的 ΔLFI,其中移植作为竞争风险。结果 我们分析了 1,093 名肝硬化门诊患者的 2,851 次就诊。虚弱严重恶化的患者基线 LFI 较差,并且更有可能患有 NAFLD、糖尿病或透析依赖。中位随访 11 个月后,整个队列中有 223 人 (20%) 死亡/因病被除名。 ΔLFI 组恶化导致死亡/退市的累积发生率增加。在根据基线 LFI、年龄、身高、MELDNa 和白蛋白进行调整的竞争风险回归中,每 3 个月 ΔLFI 变化 0.1 个单位,死亡/退市风险增加 2.04 倍(95% CI,1.35-3.09)。结论 虚弱变化与死亡/退市显着相关,与基线虚弱和 MELDNa 无关。值得注意的是,随着时间的推移,虚弱状况有所改善的患者比虚弱状况恶化的患者死亡/退市的风险更低。 我们的数据支持使用 LFI 对肝硬化患者的衰弱进行纵向测量,并为旨在逆转衰弱的介入工作奠定基础。











































 京公网安备 11010802027423号
京公网安备 11010802027423号