PLOS Medicine ( IF 10.5 ) Pub Date : 2020-03-26 , DOI: 10.1371/journal.pmed.1003079 Wayne T Steward 1 , Kimberly A Koester 1 , Mary A Guzé 1 , Valerie B Kirby 1 , Shannon M Fuller 1 , Mary E Moran 1 , Emma Wilde Botta 1 , Stuart Gaffney 1 , Corliss D Heath 2 , Steven Bromer 3 , Starley B Shade 1, 4
|
Background
The United States HIV care workforce is shrinking, which could complicate service delivery to people living with HIV (PLWH). In this study, we examined the impact of practice transformations, defined as efficiencies in structures and delivery of care, on demonstration project sites within the Workforce Capacity Building Initiative, a Health Resources and Services Administration (HRSA) Ryan White HIV/AIDS Program Special Projects of National Significance (SPNS).
Methods and findings
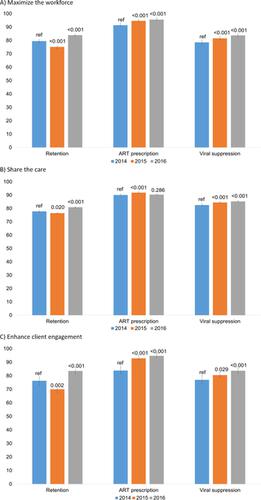
Data were collected at 14 demonstration project sites in 7 states and the District of Columbia. Organizational assessments were completed at sites once before and 4 times after implementation. They captured 3 transformation approaches: maximizing the HIV care workforce (efforts to increase the number of existing healthcare workforce members involved in the care of PLWH), share-the-care (team-based care giving more responsibility to midlevel providers and staff), and enhancing client engagement in primary HIV care to reduce emergency and inpatient care (e.g., care coordination). We also obtained Ryan White HIV/AIDS Program Services Reports (RSRs) from sites for calendar years (CYs) 2014–2016, corresponding to before, during, and after transformation. The RSR include data on client retention in HIV care, prescription of antiretroviral therapy (ART), and viral suppression. We used generalized estimating equation (GEE) models to analyze changes among sites implementing each practice transformation approach. The demonstration projects had a mean of 18.5 prescribing providers (SD = 23.5). They reported data on more than 13,500 clients per year (mean = 969/site, SD = 1,351). Demographic characteristics remained similar over time. In 2014, a majority of clients were male (71% versus 28% female and 0.2% transgender), with a mean age of 47 (interquartile range [IQR] 37–54). Racial/ethnic characteristics (48% African American, 31% Hispanic/Latino, 14% white) and HIV risk varied (31% men who have sex with men; 31% heterosexual men and women; 7% injection drug use). A substantial minority was on Medicaid (41%). Across sites, there was significant uptake in practices consistent with maximizing the HIV care workforce (18% increase, p < 0.001), share-the-care (25% increase, p < 0.001), and facilitating patient engagement in HIV primary care (13% increase, p < 0.001). There were also significant improvements over time in retention in HIV care (adjusted odds ratio [aOR] = 1.03; 95% confidence interval [CI] 1.02–1.04; p < 0.001), ART prescription levels (aOR = 1.01; 95% CI 1.00–1.01; p < 0.001), and viral suppression (aOR = 1.03; 95% CI 1.02–1.04; p < 0.001). All outcomes improved at sites that implemented transformations to maximize the HIV care workforce or improve client engagement. At sites that implemented share-the-care practices, only retention in care and viral suppression outcomes improved. Study limitations included use of demonstration project sites funded by the Ryan White HIV/AIDS Program (RWHAP), which tend to have better HIV outcomes than other US clinics; varying practice transformation designs; lack of a true control condition; and a potential Hawthorne effect because site teams were aware of the evaluation.
Conclusions
In this study, we found that practice transformations are a potential strategy for addressing anticipated workforce challenges among those providing care to PLWH. They hold the promise of optimizing the use of personnel and ensuring the delivery of care to all in need while potentially enhancing HIV care continuum outcomes.
中文翻译:

进行实践转化,以优化美国社区医疗机构中HIV初级保健的提供:一项计划实施研究。
背景
美国艾滋病毒护理人员队伍正在缩减,这可能会使向艾滋病毒携带者(PLWH)提供服务的过程变得复杂。在这项研究中,我们研究了在劳动力能力建设计划,卫生资源和服务管理局(HRSA)瑞安·怀特(Ryan White)艾滋病毒/艾滋病计划特别项目中,示范转型对示范项目现场的影响,定义为结构和医疗服务的效率国家重要性(SPNS)。
方法和发现
在7个州和哥伦比亚特区的14个示范项目现场收集了数据。实施之前和实施后4次在现场完成组织评估。他们捕获了3种转型方法:最大化HIV护理人员(努力增加参与PLWH护理的现有医护人员的数量),共享护理(基于团队的护理,使中级医疗服务提供者和员工承担更多责任),以及增加服务对象对艾滋病毒初级保健的参与,以减少急诊和住院护理(例如,护理协调)。我们还从站点获取了2014-2016日历年(CYs)的Ryan White HIV / AIDS计划服务报告(RSR),对应于改造之前,改造期间和改造之后。RSR包括有关客户在HIV护理中的保留率,抗逆转录病毒疗法(ART)的处方,和病毒抑制。我们使用广义估计方程(GEE)模型来分析实施每种实践转换方法的站点之间的变化。示范项目平均有18.5个处方提供者(SD = 23.5)。他们报告的数据超过每年13,500个客户(平均= 969 /站点,SD = 1,351)。随着时间的推移,人口特征保持相似。2014年,大多数客户是男性(71%,女性为28%,变性者为0.2%),平均年龄为47岁(四分位数间距[IQR] 37-54岁)。种族/族裔特征(48%的非洲裔美国人,31%的西班牙裔/拉丁美洲人,14%的白人)和HIV风险不同(31%与男性发生性关系的男性; 31%异性恋的男性和女性; 7%的注射毒品使用)。相当一部分人使用医疗补助(41%)。在各个网站上p <0.001),共享护理(增加25%,p <0.001)并促进患者参与HIV初级保健(增加13%,p <0.001)。随着时间的流逝,HIV护理的保留率也有了显着改善(校正比值比[aOR] = 1.03; 95%置信区间[CI] 1.02–1.04;p <0.001),ART处方水平(aOR = 1.01; 95%CI 1.00 –1.01;p <0.001)和病毒抑制(aOR = 1.03; 95%CI 1.02–1.04;p<0.001)。在实施改造以最大程度地增加艾滋病毒护理人员人数或改善服务对象参与度的地点,所有结果均得到改善。在实施共享护理实践的站点上,只有保留和病毒抑制结果有所改善。研究的局限性包括使用由瑞安·怀特(Ryan White)艾滋病计划(RWHAP)资助的示范项目地点,这些地点比美国其他诊所的艾滋病毒治疗效果更好;各种实践转换设计;缺乏真正的控制条件;以及潜在的霍索恩效应,因为现场团队已经了解了评估。
结论
在这项研究中,我们发现实践转变是一种潜在的策略,可以解决为PLWH提供护理的员工中预期的劳动力挑战。他们承诺优化人员使用并确保向所有需要的人提供护理,同时潜在地提高艾滋病毒护理的连续性成果。











































 京公网安备 11010802027423号
京公网安备 11010802027423号