当前位置:
X-MOL 学术
›
Cancer Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Early variations in lymphocytes and T lymphocyte subsets are associated with radiation pneumonitis in lung cancer patients and experimental mice received thoracic irradiation.
Cancer Medicine ( IF 4 ) Pub Date : 2020-03-24 , DOI: 10.1002/cam4.2987 Pu Zhou 1 , Lu Chen 1 , Dong Yan 2 , Changlin Huang 1 , Guangpeng Chen 1 , Zhiyi Wang 1 , Liangzhi Zhong 1 , Wen Luo 1 , Diangang Chen 1 , Chui Chun 3 , Shushu Zhang 3 , Guanghui Li 1
Cancer Medicine ( IF 4 ) Pub Date : 2020-03-24 , DOI: 10.1002/cam4.2987 Pu Zhou 1 , Lu Chen 1 , Dong Yan 2 , Changlin Huang 1 , Guangpeng Chen 1 , Zhiyi Wang 1 , Liangzhi Zhong 1 , Wen Luo 1 , Diangang Chen 1 , Chui Chun 3 , Shushu Zhang 3 , Guanghui Li 1
Affiliation
|
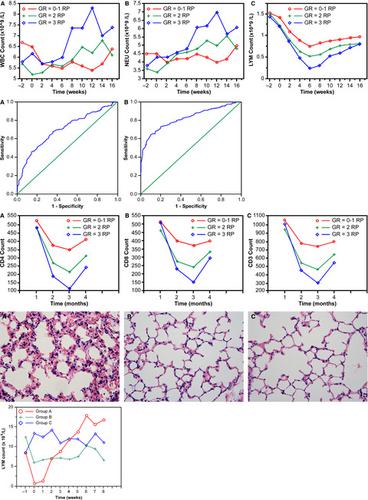
There were no ideal markers to predict the development of radiation pneumonitis (RP). We want to investigate the value of variations of lymphocytes and T lymphocyte subsets in predicting RP after radiotherapy (RT) of lung cancer based on previous clinical findings. A total of 182 lung cancer patients who received RT were retrospectively analyzed. Circulating lymphocytes and T lymphocyte subsets were measured before, during, and after RT. Patients were evaluated from the start of RT to 6 months post-RT. A mice model with acute radiation-induced lung injury was established and circulating lymphocytes were measured weekly until 8 weeks after irradiation. Univariate and multivariate analyses were adopted to identify risk factors of RP. Lymphocyte levels significantly decreased (P < .001) in patients before RP symptoms developed that also was able to be seen in the mice model and the values recovered during remission of symptoms. The decrease in lymphocyte count reflected the severity of RP. Meanwhile, CD4+ T lymphocyte count was significantly lower during the occurrence of symptoms in patients with RP than in those without RP (P < .001), and it improved along with RP recovery. Levels of lymphocytes and CD4+ T lymphocyte subsets proved as independent predictors of RP. Here we showed that lower peripheral blood levels of lymphocytes and CD4+ T lymphocyte were associated with an increased risk of RP, which was validated by this mice model, and thus are associated with differences in radiation-induced lung toxicity among individuals and help identify those who are susceptible to developing RP after RT.
中文翻译:

淋巴细胞和 T 淋巴细胞亚群的早期变异与肺癌患者和接受胸部照射的实验小鼠的放射性肺炎有关。
没有理想的标志物来预测放射性肺炎 (RP) 的发展。我们想根据既往的临床发现,研究淋巴细胞和 T 淋巴细胞亚群的变化在预测肺癌放疗 (RT) 后 RP 中的价值。对 182 名接受放疗的肺癌患者进行了回顾性分析。在 RT 之前、期间和之后测量循环淋巴细胞和 T 淋巴细胞亚群。从放疗开始到放疗后 6 个月对患者进行评估。建立急性放射诱导肺损伤小鼠模型,每周测量循环淋巴细胞,直至照射后 8 周。采用单变量和多变量分析来确定RP的危险因素。淋巴细胞水平显着降低(P < . 001) 在 RP 症状出现之前的患者中,这也能够在小鼠模型中看到,并且在症状缓解期间恢复了值。淋巴细胞计数的减少反映了 RP 的严重程度。同时,RP患者出现症状期间CD4+ T淋巴细胞计数明显低于无RP患者(P < .001),并且随着RP的恢复而改善。淋巴细胞和 CD4+ T 淋巴细胞亚群的水平被证明是 RP 的独立预测因子。在这里,我们发现淋巴细胞和 CD4+ T 淋巴细胞的外周血水平较低与 RP 风险增加有关,这一点得到了该小鼠模型的验证,因此与个体之间辐射诱导的肺毒性的差异有关,并有助于识别那些RT 后容易发生 RP。
更新日期:2020-03-24
中文翻译:

淋巴细胞和 T 淋巴细胞亚群的早期变异与肺癌患者和接受胸部照射的实验小鼠的放射性肺炎有关。
没有理想的标志物来预测放射性肺炎 (RP) 的发展。我们想根据既往的临床发现,研究淋巴细胞和 T 淋巴细胞亚群的变化在预测肺癌放疗 (RT) 后 RP 中的价值。对 182 名接受放疗的肺癌患者进行了回顾性分析。在 RT 之前、期间和之后测量循环淋巴细胞和 T 淋巴细胞亚群。从放疗开始到放疗后 6 个月对患者进行评估。建立急性放射诱导肺损伤小鼠模型,每周测量循环淋巴细胞,直至照射后 8 周。采用单变量和多变量分析来确定RP的危险因素。淋巴细胞水平显着降低(P < . 001) 在 RP 症状出现之前的患者中,这也能够在小鼠模型中看到,并且在症状缓解期间恢复了值。淋巴细胞计数的减少反映了 RP 的严重程度。同时,RP患者出现症状期间CD4+ T淋巴细胞计数明显低于无RP患者(P < .001),并且随着RP的恢复而改善。淋巴细胞和 CD4+ T 淋巴细胞亚群的水平被证明是 RP 的独立预测因子。在这里,我们发现淋巴细胞和 CD4+ T 淋巴细胞的外周血水平较低与 RP 风险增加有关,这一点得到了该小鼠模型的验证,因此与个体之间辐射诱导的肺毒性的差异有关,并有助于识别那些RT 后容易发生 RP。



























 京公网安备 11010802027423号
京公网安备 11010802027423号