JAMA Surgery ( IF 15.7 ) Pub Date : 2020-05-01 , DOI: 10.1001/jamasurg.2020.0024 Alfred C Kuo 1, 2 , Nicholas J Giori 3 , Thomas R Bowe 4 , Luisa Manfredi 4 , Narlina F Lalani 5 , David A Nordin 5 , Alex H S Harris 4
|
Importance The minimal clinically important difference (MCID) in a patient-reported outcome measure (PROM) is the smallest change that patients perceive as beneficial. Accurate MCIDs are required when PROMs are used to evaluate the value of surgical interventions.
Objective To use well-defined distribution-based and anchor-based methods to calculate MCIDs in the Hip Disability and Osteoarthritis Outcome Score (HOOS) and in the Knee Injury and Osteoarthritis Outcome Score (KOOS) for veterans undergoing primary total hip arthroplasty or total knee arthroplasty.
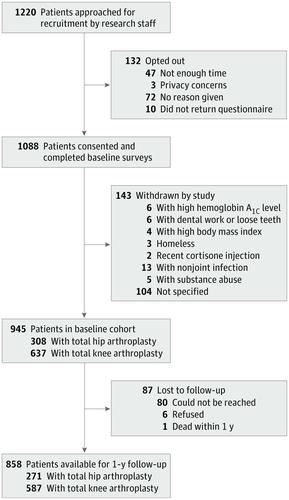
Design, Setting, and Participants A prospective cohort study was conducted of 858 patients undergoing total joint replacement between March 16, 2015, and March 9, 2017, at 3 high-complexity Veterans Affairs Medical Centers.
Interventions Patients undergoing total hip arthroplasty or total knee arthroplasty were administered HOOS or KOOS PROMs prior to and 1 year after surgery. The Self-Administered Patient Satisfaction Scale (SAPS) for primary hip or knee arthroplasty was administered at 1-year follow-up as an anchor PROM.
Main Outcomes and Measures The HOOS and KOOS before and 1 year after surgery, change scores (difference between postoperative and preoperative PROM scores), and MCIDs for each measure. For anchor-based methods, receiver operating characteristic curve analysis was performed, including calculation of the area under the curve.
Results The mean (SD) age of the 271 patients who underwent hip arthroplasty was 65.6 (8.3) years, and the mean (SD) age of the 587 patients who underwent knee arthroplasty was 66.1 (8.2) years. There were 547 men in the knee arthroplasty cohort and 256 men in the hip arthroplasty cohort (total, 803 men). There were significant improvements in the mean values of every PROM, with mean (SD) differences greater than 39 for HOOS Joint Replacement (JR) and every hip subscale (HOOS JR, 39.7 [20.2]; pain, 47.6 [20.5]; symptoms, 45.1 [21.5]; activities of daily living, 43.7 [22.1]; recreation, 49.2 [33.5]; quality of life, 50.3 [27.8]) and mean (SD) differences greater than 29 for KOOS JR and every knee subscale (KOOS JR, 30.4 [17.5]; pain, 38.0 [20.4]; symptoms, 29.5 [22.1]; activities of daily living, 34.8 [20.5]; recreation, 34.6 [31.1]; quality of life, 35.2 [26.8]). Different calculation methods yielded a wide range of MCIDs. Distribution-based approaches tended to give lower values than the anchor-based approaches, which gave similar values for most PROMs. Area under the curve values demonstrated good to excellent discrimination for SAPS for nearly all PROMs.
Conclusions and Relevance Minimal clinically important difference estimates can be highly variable depending on the method used. Patient satisfaction measured by SAPS is a suitable anchor for the HOOS and KOOS. This study suggests that the SAPS-anchored MCID values presented here be used in future studies of total hip arthroplasty and total knee arthroplasty for veterans.
中文翻译:

在退伍军人卫生管理局医院中,为进行全髋关节或膝关节置换术的退伍军人患者报告的结果衡量标准中确定最小的临床重要差异的比较方法。
重要性 患者报告的结局指标(PROM)中最小的临床重要差异(MCID)是患者认为有益的最小变化。当使用PROM评估手术干预的价值时,需要准确的MCID。
目的 使用明确定义的基于分布和基于锚的方法来计算进行初次全髋关节置换术或全膝关节退伍军人的髋关节残疾和骨关节炎结果评分(HOOS)以及膝关节损伤和骨关节炎结果评分(KOOS)的MCID关节置换术。
Design, Setting, and Participants A prospective cohort study was conducted of 858 patients undergoing total joint replacement between March 16, 2015, and March 9, 2017, at 3 high-complexity Veterans Affairs Medical Centers.
Interventions Patients undergoing total hip arthroplasty or total knee arthroplasty were administered HOOS or KOOS PROMs prior to and 1 year after surgery. The Self-Administered Patient Satisfaction Scale (SAPS) for primary hip or knee arthroplasty was administered at 1-year follow-up as an anchor PROM.
Main Outcomes and Measures The HOOS and KOOS before and 1 year after surgery, change scores (difference between postoperative and preoperative PROM scores), and MCIDs for each measure. For anchor-based methods, receiver operating characteristic curve analysis was performed, including calculation of the area under the curve.
Results 271例行髋关节置换术的患者的平均(SD)年龄为65.6(8.3)岁,而587例行膝关节置换术的患者的平均(SD)年龄为66.1(8.2)岁。膝关节置换队列中有547名男性,髋关节置换队列中有256名男性(总计803名男性)。每个PROM的平均值都有显着改善,HOOS关节置换(JR)和每个髋关节量表的平均(SD)差异均大于39(HOOS JR,39.7 [20.2];疼痛,47.6 [20.5];症状, 45.1 [21.5];日常生活活动43.7 [22.1];娱乐活动49.2 [33.5];生活质量50.3 [27.8])和KOOS JR和每个膝盖分量表的平均(SD)差异均大于29(KOOS JR ,30.4 [17.5];疼痛,38.0 [20.4];症状,29.5 [22.1];日常生活活动,34.8 [20.5];娱乐,34.6 [31.1];生活质量,35。2 [26.8])。不同的计算方法产生了各种各样的MCID。与基于锚的方法相比,基于分布的方法倾向于提供较低的值,而基于锚的方法对于大多数PROM都具有相似的值。曲线值下的面积对于几乎所有PROM都显示出对SAPS的良好至出色的区分。
结论和相关性 根据所使用的方法,最小的临床重要差异估计值可能会高度可变。SAPS评估的患者满意度是HOOS和KOOS的合适锚点。这项研究表明,此处介绍的SAPS锚定的MCID值可用于退伍军人的全髋关节置换术和全膝关节置换术的未来研究中。











































 京公网安备 11010802027423号
京公网安备 11010802027423号