Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Prevalence and Outcomes of Infection Among Patients in Intensive Care Units in 2017
JAMA ( IF 63.1 ) Pub Date : 2020-04-21 , DOI: 10.1001/jama.2020.2717 Jean-Louis Vincent 1 , Yasser Sakr 2 , Mervyn Singer 3 , Ignacio Martin-Loeches 4, 5 , Flavia R Machado 6 , John C Marshall 7 , Simon Finfer 8 , Paolo Pelosi 9, 10 , Luca Brazzi 11 , Dita Aditianingsih 12 , Jean-François Timsit 13 , Bin Du 14 , Xavier Wittebole 15 , Jan Máca 16 , Santhana Kannan 17 , Luis A Gorordo-Delsol 18 , Jan J De Waele 19 , Yatin Mehta 20 , Marc J M Bonten 21 , Ashish K Khanna 22, 23 , Marin Kollef 24 , Mariesa Human 25 , Derek C Angus 26 ,
JAMA ( IF 63.1 ) Pub Date : 2020-04-21 , DOI: 10.1001/jama.2020.2717 Jean-Louis Vincent 1 , Yasser Sakr 2 , Mervyn Singer 3 , Ignacio Martin-Loeches 4, 5 , Flavia R Machado 6 , John C Marshall 7 , Simon Finfer 8 , Paolo Pelosi 9, 10 , Luca Brazzi 11 , Dita Aditianingsih 12 , Jean-François Timsit 13 , Bin Du 14 , Xavier Wittebole 15 , Jan Máca 16 , Santhana Kannan 17 , Luis A Gorordo-Delsol 18 , Jan J De Waele 19 , Yatin Mehta 20 , Marc J M Bonten 21 , Ashish K Khanna 22, 23 , Marin Kollef 24 , Mariesa Human 25 , Derek C Angus 26 ,
Affiliation
|
Importance
Infection is frequent among patients in the intensive care unit (ICU). Contemporary information about the types of infections, causative pathogens, and outcomes can aid the development of policies for prevention, diagnosis, treatment, and resource allocation and may assist in the design of interventional studies. Objective
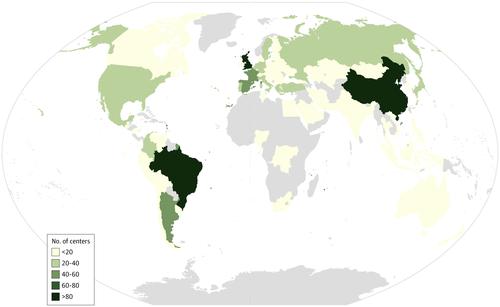
To provide information about the prevalence and outcomes of infection and the available resources in ICUs worldwide. Design, Setting, and Participants
Observational 24-hour point prevalence study with longitudinal follow-up at 1150 centers in 88 countries. All adult patients (aged ≥18 years) treated at a participating ICU during a 24-hour period commencing at 08:00 on September 13, 2017, were included. The final follow-up date was November 13, 2017. Exposures
Infection diagnosis and receipt of antibiotics. Main Outcomes and Measures
Prevalence of infection and antibiotic exposure (cross-sectional design) and all-cause in-hospital mortality (longitudinal design). Results
Among 15 202 included patients (mean age, 61.1 years [SD, 17.3 years]; 9181 were men [60.4%]), infection data were available for 15 165 (99.8%); 8135 (54%) had suspected or proven infection, including 1760 (22%) with ICU-acquired infection. A total of 10 640 patients (70%) received at least 1 antibiotic. The proportion of patients with suspected or proven infection ranged from 43% (141/328) in Australasia to 60% (1892/3150) in Asia and the Middle East. Among the 8135 patients with suspected or proven infection, 5259 (65%) had at least 1 positive microbiological culture; gram-negative microorganisms were identified in 67% of these patients (n = 3540), gram-positive microorganisms in 37% (n = 1946), and fungal microorganisms in 16% (n = 864). The in-hospital mortality rate was 30% (2404/7936) in patients with suspected or proven infection. In a multilevel analysis, ICU-acquired infection was independently associated with higher risk of mortality compared with community-acquired infection (odds ratio [OR], 1.32 [95% CI, 1.10-1.60]; P = .003). Among antibiotic-resistant microorganisms, infection with vancomycin-resistant Enterococcus (OR, 2.41 [95% CI, 1.43-4.06]; P = .001), Klebsiella resistant to β-lactam antibiotics, including third-generation cephalosporins and carbapenems (OR, 1.29 [95% CI, 1.02-1.63]; P = .03), or carbapenem-resistant Acinetobacter species (OR, 1.40 [95% CI, 1.08-1.81]; P = .01) was independently associated with a higher risk of death vs infection with another microorganism. Conclusions and Relevance
In a worldwide sample of patients admitted to ICUs in September 2017, the prevalence of suspected or proven infection was high, with a substantial risk of in-hospital mortality.
中文翻译:

2017 年重症监护病房患者的感染流行率和结局
重症监护病房 (ICU) 的患者中感染很常见。有关感染类型、致病病原体和结果的当代信息有助于制定预防、诊断、治疗和资源分配政策,并可能有助于干预研究的设计。目的 提供有关感染的流行率和结果以及全球 ICU 可用资源的信息。设计、设置和参与者在 88 个国家的 1150 个中心进行纵向随访的 24 小时观察点患病率研究。纳入了从 2017 年 9 月 13 日 08:00 开始的 24 小时内在参与的 ICU 接受治疗的所有成年患者(年龄≥18 岁)。最终随访日期为 2017 年 11 月 13 日。 暴露 感染诊断和抗生素接收。主要结果和措施 感染率和抗生素暴露率(横断面设计)和全因住院死亡率(纵向设计)。结果 在 15 202 名患者中(平均年龄 61.1 岁 [SD,17.3 岁];9181 名男性 [60.4%]),可获得 15 165 名(99.8%)的感染数据;8135 人(54%)怀疑或证实感染,其中 1760 人(22%)患有 ICU 获得性感染。共有 10 640 名患者 (70%) 接受了至少一种抗生素。疑似或确诊感染的患者比例从大洋洲的 43% (141/328) 到亚洲和中东的 60% (1892/3150) 不等。在疑似或确诊感染的 8135 名患者中,5259 名(65%)至少有 1 次微生物培养阳性;67% 的患者(n = 3540)发现了革兰氏阴性微生物,革兰氏阳性微生物占 37% (n = 1946),真菌微生物占 16% (n = 864)。疑似或确诊感染患者的住院死亡率为 30% (2404/7936)。在一项多水平分析中,与社区获得性感染相比,ICU 获得性感染与更高的死亡风险独立相关(比值比 [OR],1.32 [95% CI,1.10-1.60];P = .003)。在抗生素耐药微生物中,耐万古霉素肠球菌感染(OR,2.41 [95% CI,1.43-4.06];P = .001),对 β-内酰胺类抗生素(包括第三代头孢菌素和碳青霉烯类)耐药的克雷伯菌(OR, 1.29 [95% CI, 1.02-1.63]; P = .03) 或耐碳青霉烯类不动杆菌 (OR, 1.40 [95% CI, 1.08-1.81]; P = .01) 与较高的死亡与感染另一种微生物。
更新日期:2020-04-21
中文翻译:

2017 年重症监护病房患者的感染流行率和结局
重症监护病房 (ICU) 的患者中感染很常见。有关感染类型、致病病原体和结果的当代信息有助于制定预防、诊断、治疗和资源分配政策,并可能有助于干预研究的设计。目的 提供有关感染的流行率和结果以及全球 ICU 可用资源的信息。设计、设置和参与者在 88 个国家的 1150 个中心进行纵向随访的 24 小时观察点患病率研究。纳入了从 2017 年 9 月 13 日 08:00 开始的 24 小时内在参与的 ICU 接受治疗的所有成年患者(年龄≥18 岁)。最终随访日期为 2017 年 11 月 13 日。 暴露 感染诊断和抗生素接收。主要结果和措施 感染率和抗生素暴露率(横断面设计)和全因住院死亡率(纵向设计)。结果 在 15 202 名患者中(平均年龄 61.1 岁 [SD,17.3 岁];9181 名男性 [60.4%]),可获得 15 165 名(99.8%)的感染数据;8135 人(54%)怀疑或证实感染,其中 1760 人(22%)患有 ICU 获得性感染。共有 10 640 名患者 (70%) 接受了至少一种抗生素。疑似或确诊感染的患者比例从大洋洲的 43% (141/328) 到亚洲和中东的 60% (1892/3150) 不等。在疑似或确诊感染的 8135 名患者中,5259 名(65%)至少有 1 次微生物培养阳性;67% 的患者(n = 3540)发现了革兰氏阴性微生物,革兰氏阳性微生物占 37% (n = 1946),真菌微生物占 16% (n = 864)。疑似或确诊感染患者的住院死亡率为 30% (2404/7936)。在一项多水平分析中,与社区获得性感染相比,ICU 获得性感染与更高的死亡风险独立相关(比值比 [OR],1.32 [95% CI,1.10-1.60];P = .003)。在抗生素耐药微生物中,耐万古霉素肠球菌感染(OR,2.41 [95% CI,1.43-4.06];P = .001),对 β-内酰胺类抗生素(包括第三代头孢菌素和碳青霉烯类)耐药的克雷伯菌(OR, 1.29 [95% CI, 1.02-1.63]; P = .03) 或耐碳青霉烯类不动杆菌 (OR, 1.40 [95% CI, 1.08-1.81]; P = .01) 与较高的死亡与感染另一种微生物。











































 京公网安备 11010802027423号
京公网安备 11010802027423号