Modern Pathology ( IF 7.1 ) Pub Date : 2020-03-20 , DOI: 10.1038/s41379-020-0524-1 Basile Tessier-Cloutier 1, 2 , Kim E Kortekaas 3 , Emily Thompson 2 , Jennifer Pors 1, 2 , Julia Chen 2 , Julie Ho 2 , Leah M Prentice 4 , Melissa K McConechy 4 , Christine Chow 5 , Lily Proctor 6 , Jessica N McAlpine 6 , David G Huntsman 2, 5, 7 , C Blake Gilks 1, 2, 5 , Tjalling Bosse 8 , Lynn N Hoang 1, 2, 5
|
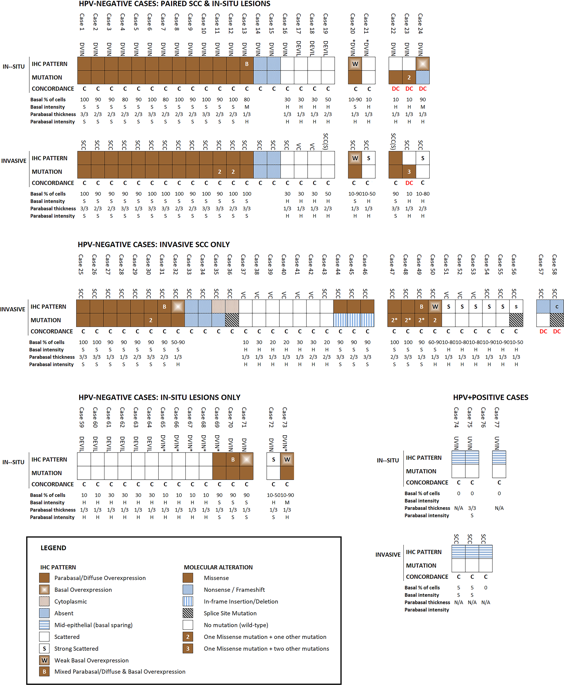
The recent literature has shown that vulvar squamous cell carcinoma (VSCC) can be stratified into two prognostically relevant groups based on human papillomavirus (HPV) status. The prognostic value of p53 for further sub-stratification, particularly in the HPV-independent group, has not been agreed upon. This disagreement is likely due to tremendous variations in p53 immunohistochemical (IHC) interpretation. To address this problem, we sought to compare p53 IHC patterns with TP53 mutation status. We studied 61 VSCC (48 conventional VSCC, 2 VSCC with sarcomatoid features, and 11 verrucous carcinomas) and 42 in situ lesions (30 differentiated vulvar intraepithelial neoplasia [dVIN], 9 differentiated exophytic vulvar intraepithelial lesions [deVIL], and 3 high-grade squamous intraepithelial lesions or usual vulvar intraepithelial neoplasia [HSIL/uVIN]). IHC for p16 and p53, and sequencing of TP53 exons 4–9 were performed. HPV in situ hybridization (ISH) was performed in selected cases. We identified six major p53 IHC patterns, two wild-type patterns: (1) scattered, (2) mid-epithelial expression (with basal sparing), and four mutant patterns: (3) basal overexpression, (4) parabasal/diffuse overexpression, (5) absent, and (6) cytoplasmic expression. These IHC patterns were consistent with TP53 mutation status in 58/61 (95%) VSCC and 39/42 (93%) in situ lesions. Cases that exhibited strong scattered staining and those with a weak basal overexpression pattern could be easily confused. The mid-epithelial pattern was exclusively observed in p16-positive lesions; the basal and parabasal layers that had absent p53 staining, appeared to correlate with the cells that were positive for HPV-ISH. This study describes a pattern-based p53 IHC interpretation framework, which can be utilized as a surrogate marker for TP53 mutational status in both VSCC and vulvar in situ lesions.
中文翻译:

外阴原位和浸润性鳞状细胞癌的主要 p53 免疫组织化学模式以及与 TP53 突变状态的相关性。
最近的文献表明,外阴鳞状细胞癌 (VSCC) 可以根据人乳头瘤病毒 (HPV) 状态分为两个预后相关的组。p53 对进一步亚分层的预后价值,特别是在 HPV 独立组中的预后价值尚未达成一致。这种分歧可能是由于 p53 免疫组织化学 (IHC) 解释的巨大差异。为了解决这个问题,我们试图将 p53 IHC 模式与TP53进行比较突变状态。我们研究了 61 个 VSCC(48 个常规 VSCC,2 个具有肉瘤样特征的 VSCC,和 11 个疣状癌)和 42 个原位病变(30 个分化的外阴上皮内瘤变 [dVIN],9 个分化的外生性外阴上皮内病变 [deVIL],和 3 个高级别鳞状上皮内病变或常见的外阴上皮内瘤变 [HSIL/uVIN])。对 p16 和 p53 进行了 IHC,并对TP53外显子 4-9 进行了测序。在选定的病例中进行了 HPV 原位杂交 (ISH)。我们确定了六种主要的 p53 IHC 模式,两种野生型模式:(1) 分散型,(2) 中上皮表达(具有基底保留),以及四种突变模式:(3) 基底过度表达,(4) 副基底/弥散过度表达,(5) 缺失,和 (6) 细胞质表达。这些 IHC 模式与58/61 (95%) VSCC 和 39/42 (93%) 原位病变中的TP53突变状态。表现出强烈散在染色的病例和具有弱基础过度表达模式的病例很容易混淆。中层上皮模式仅在 p16 阳性病变中观察到;没有 p53 染色的基底层和副基底层似乎与 HPV-ISH 阳性细胞相关。本研究描述了一种基于模式的 p53 IHC 解释框架,可用作VSCC 和外阴原位病变中TP53突变状态的替代标记。











































 京公网安备 11010802027423号
京公网安备 11010802027423号