Clinical Gastroenterology and Hepatology ( IF 11.6 ) Pub Date : 2020-03-20 , DOI: 10.1016/j.cgh.2020.03.039 Ming-Han Chen , Ming-Huang Chen , Chung-Tei Chou , Ming-Chih Hou , Chang-Youh Tsai , Yi-Hsiang Huang
|
Background & Aims
In patients who have resolved hepatitis B virus (HBV) infection, treatment of rheumatoid arthritis (RA) can result in reappearance of hepatitis B surface antigen (HBsAg), called reverse seroconversion. We investigated clinical features and outcomes of reverse seroconversion in patients who received immunosuppressant or biologic therapy for RA.
Methods
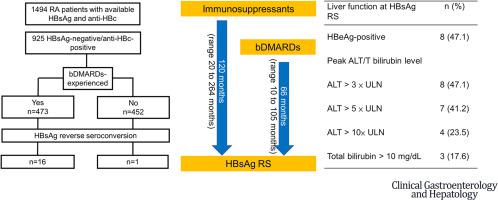
We identified 1494 patients with RA (925 who resolved HBV infection) and available data on levels of antibody to HB core antigen and HBsAg who had attended Taipei Veterans General Hospital from January 2007 through December 2017. We identified 17 cases (median age, 66 years) who were negative for HBsAg before treatment of RA and reverse seroconversion (HBsAg reappearance) after glucocorticoid treatment (n = 13) and/or biologic therapy (adalimumab, n = 2; etanercept, n = 1; rituximab, n = 9; or abatacept, n = 4). Four patients were positive for antibodies against HBsAg (seroconverted) before the immunosuppressive treatment.
Results
The median time from immunosuppressive treatment to reverse seroconversion was 120 months (range, 20–264 months), whereas the time from biologic therapy treatment to reverse seroconversion was 66 months (range, 10–105 months). After reverse seroconversion, 8 individuals (47.1%) were positive for HB e antigen; 9 cases (52.9%) did not have a flare of alanine transaminase. However, 3 patients (17.6%) developed liver decompensation.
Conclusions
In patients who resolved HBV infection and received immunosuppressant treatment of RA, risk of reversal of seroconversion is low but persists for up to 10 years. Patients with RA who previously resolved HBV infections should be monitored for levels of HBsAg and HBV DNA once immunosuppressive treatment of RA begins.
中文翻译:

接受免疫抑制治疗的类风湿性关节炎患者血清转化逆转的风险低但持久。
背景与目标
在乙型肝炎病毒 (HBV) 感染已解决的患者中,类风湿性关节炎 (RA) 的治疗可导致乙型肝炎表面抗原 (HBsAg) 重新出现,称为反向血清转换。我们调查了接受免疫抑制剂或生物制剂治疗的 RA 患者血清逆转的临床特征和结果。
方法
我们确定了 2007 年 1 月至 2017 年 12 月在台北退伍军人总医院就诊的 1494 名 RA 患者(925 名治愈了 HBV 感染)以及有关 HB 核心抗原和 HBsAg 抗体水平的可用数据。我们确定了 17 例病例(中位年龄,66 岁) ) RA 治疗前 HBsAg 阴性且糖皮质激素治疗 (n = 13) 和/或生物疗法(阿达木单抗,n = 2;依那西普,n = 1;利妥昔单抗,n = 9;或阿巴西普,n = 4)。4 名患者在免疫抑制治疗前对 HBsAg 抗体呈阳性(血清转化)。
结果
从免疫抑制治疗到逆转血清转换的中位时间为 120 个月(范围,20-264 个月),而从生物治疗治疗到逆转血清转换的时间为 66 个月(范围,10-105 个月)。血清逆转后,8人(47.1%)HBe抗原阳性;9 例 (52.9%) 未出现丙氨酸转氨酶异常。然而,3 名患者 (17.6%) 出现肝功能失代偿。
结论
在治愈 HBV 感染并接受 RA 免疫抑制剂治疗的患者中,血清转化逆转的风险较低,但持续时间长达 10 年。一旦开始对 RA 进行免疫抑制治疗,应监测先前已治愈 HBV 感染的 RA 患者的 HBsAg 和 HBV DNA 水平。









































 京公网安备 11010802027423号
京公网安备 11010802027423号