当前位置:
X-MOL 学术
›
Cancer Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Investigating association of perineural invasion on prostate biopsy with Gleason score upgrading at prostatectomy: A multi-institutional analysis.
Cancer Medicine ( IF 2.9 ) Pub Date : 2020-03-18 , DOI: 10.1002/cam4.2920 Andrew R Barsky 1 , Ryan D Kraus 2 , Ruben Carmona 1 , Patricia M G Santos 3 , Carrie Li 1 , Lauren E Schwartz 4 , Leslie K Ballas 5 , Neha Vapiwala 1
Cancer Medicine ( IF 2.9 ) Pub Date : 2020-03-18 , DOI: 10.1002/cam4.2920 Andrew R Barsky 1 , Ryan D Kraus 2 , Ruben Carmona 1 , Patricia M G Santos 3 , Carrie Li 1 , Lauren E Schwartz 4 , Leslie K Ballas 5 , Neha Vapiwala 1
Affiliation
|
BACKGROUND
The significance of perineural invasion (PNI) in prostate cancer (PC) is unclear. A recent report of patients with pT2N0R0 PC found that PNI at prostatectomy was independently associated with higher Gleason score and more diffuse prostatic disease. We aimed to test our hypothesis that PNI on prostate biopsy in pT2N0R0 patients is associated with increased Gleason score upgrading at prostatectomy.
METHODS
We identified 2892 patients status post prostatectomy with pT2N0R0 PC from three institutions, diagnosed between 1 January 2008 and 31 December 2014. Multivariable logistic regression (MVA) was used to evaluate the association between prostate biopsy PNI status and surgical Gleason upgrading, while controlling for potential confounders.
RESULTS
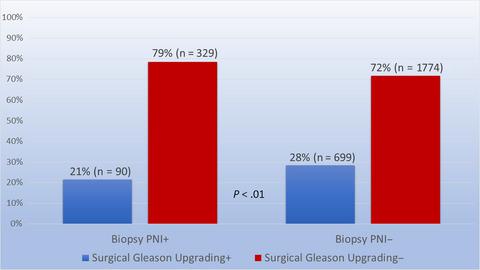
Of the 2892 patients identified, 14% had PNI on biopsy, of whom 21% had surgical Gleason upgrading, while 28% without PNI on biopsy had such upgrading (P < .01). On MVA, the odds ratio (OR) of surgical Gleason upgrading for patients with biopsy PNI relative to patients without biopsy PNI was 0.69 (P < .01). The variables associated with surgical Gleason upgrading were age ≤60 years (OR 1.22, P = .02) and preoperative PSA >4 ng/mL (OR 1.26, P = .02).
CONCLUSIONS
In post-prostatectomy patients with favorable-risk PC, PNI on prostate biopsy was not associated with surgical Gleason score upgrading. This may be due to the association of PNI with more diffuse disease, leading to increased biopsy tumor yield and grading accuracy. These findings suggest that in this setting, biopsy PNI alone should not be a concern for more aggressive disease requiring pathologic confirmation or intervention. This may help guide treatment decision-making for men debating active surveillance, radiation, and surgery.
中文翻译:

调查前列腺活检中神经周围浸润与前列腺切除术 Gleason 评分升级的关联:一项多机构分析。
背景 前列腺癌 (PC) 中神经周围浸润 (PNI) 的意义尚不清楚。最近一份关于 pT2N0R0 PC 患者的报告发现,前列腺切除术中的 PNI 与较高的 Gleason 评分和更弥漫的前列腺疾病独立相关。我们的目的是检验我们的假设,即 pT2N0R0 患者前列腺活检的 PNI 与前列腺切除术时 Gleason 评分升级增加有关。方法 我们确定了 2892 名来自三个机构的 pT2N0R0 PC 前列腺切除术后患者,诊断时间为 2008 年 1 月 1 日至 2014 年 12 月 31 日。多变量逻辑回归 (MVA) 用于评估前列腺活检 PNI 状态与手术格里森升级之间的关联,同时控制潜在的混杂因素。结果 在确定的 2892 名患者中,14% 的活检显示 PNI,其中 21% 进行了外科格里森升级,而 28% 活检未进行 PNI 升级(P < .01)。在 MVA 上,有活检 PNI 的患者与没有活检 PNI 的患者相比,手术格里森升级的优势比 (OR) 为 0.69 (P < .01)。与手术格里森升级相关的变量是年龄≤60 岁(OR 1.22,P = .02)和术前 PSA >4 ng/mL(OR 1.26,P = .02)。结论 在具有有利风险 PC 的前列腺切除术后患者中,前列腺活检的 PNI 与手术 Gleason 评分升级无关。这可能是由于 PNI 与更广泛的疾病相关,导致活检肿瘤产量和分级准确性增加。这些发现表明,在这种情况下,对于需要病理证实或干预的更具侵袭性的疾病,不应单独使用活检 PNI。
更新日期:2020-03-18
中文翻译:

调查前列腺活检中神经周围浸润与前列腺切除术 Gleason 评分升级的关联:一项多机构分析。
背景 前列腺癌 (PC) 中神经周围浸润 (PNI) 的意义尚不清楚。最近一份关于 pT2N0R0 PC 患者的报告发现,前列腺切除术中的 PNI 与较高的 Gleason 评分和更弥漫的前列腺疾病独立相关。我们的目的是检验我们的假设,即 pT2N0R0 患者前列腺活检的 PNI 与前列腺切除术时 Gleason 评分升级增加有关。方法 我们确定了 2892 名来自三个机构的 pT2N0R0 PC 前列腺切除术后患者,诊断时间为 2008 年 1 月 1 日至 2014 年 12 月 31 日。多变量逻辑回归 (MVA) 用于评估前列腺活检 PNI 状态与手术格里森升级之间的关联,同时控制潜在的混杂因素。结果 在确定的 2892 名患者中,14% 的活检显示 PNI,其中 21% 进行了外科格里森升级,而 28% 活检未进行 PNI 升级(P < .01)。在 MVA 上,有活检 PNI 的患者与没有活检 PNI 的患者相比,手术格里森升级的优势比 (OR) 为 0.69 (P < .01)。与手术格里森升级相关的变量是年龄≤60 岁(OR 1.22,P = .02)和术前 PSA >4 ng/mL(OR 1.26,P = .02)。结论 在具有有利风险 PC 的前列腺切除术后患者中,前列腺活检的 PNI 与手术 Gleason 评分升级无关。这可能是由于 PNI 与更广泛的疾病相关,导致活检肿瘤产量和分级准确性增加。这些发现表明,在这种情况下,对于需要病理证实或干预的更具侵袭性的疾病,不应单独使用活检 PNI。











































 京公网安备 11010802027423号
京公网安备 11010802027423号