当前位置:
X-MOL 学术
›
Exp. Mol. Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
The impact of bacteria-derived ultrafine dust particles on pulmonary diseases.
Experimental & Molecular Medicine ( IF 9.5 ) Pub Date : 2020-03-17 , DOI: 10.1038/s12276-019-0367-3 Jinho Yang 1, 2 , Eun Kyoung Kim 1 , Hyeon Ju Park 1 , Andrea McDowell 1 , Yoon-Keun Kim 1
Experimental & Molecular Medicine ( IF 9.5 ) Pub Date : 2020-03-17 , DOI: 10.1038/s12276-019-0367-3 Jinho Yang 1, 2 , Eun Kyoung Kim 1 , Hyeon Ju Park 1 , Andrea McDowell 1 , Yoon-Keun Kim 1
Affiliation
|
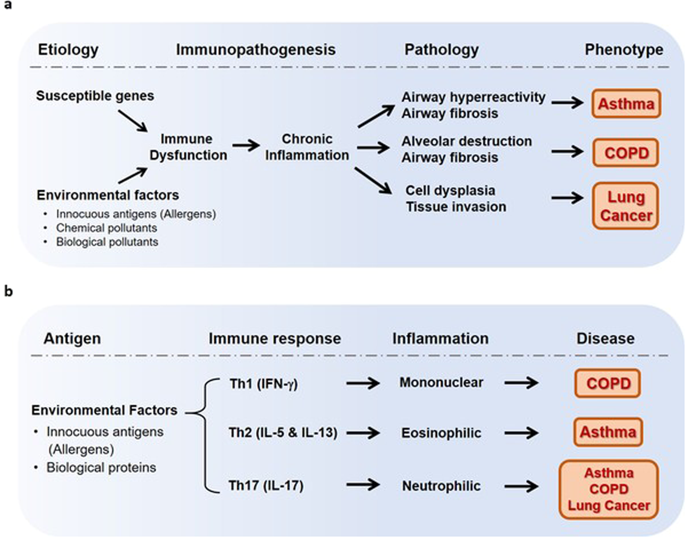
The relationship between ambient particulate matter exposure and health has been well established. Ultrafine particles (UFP) with a diameter of 100 nm or less are known to increase pulmonary disease risk. Biological factors in dust containing UFP can cause severe inflammatory reactions. Pulmonary diseases develop primarily as a result of chronic inflammation caused by immune dysfunction. Thus, this review focuses on the adverse pulmonary effects of biological UFP, principally lipopolysaccharide (LPS), and bacterial extracellular vesicles (EVs), in indoor dust and the pathophysiological mechanisms involved in the development of chronic pulmonary diseases. The impact of LPS-induced pulmonary inflammation is based primarily on the amount of inhaled LPS. When relatively low levels of LPS are inhaled, a cascade of immune responses leads to Th2 cell induction, and IL-5 and IL-13 released by Th2 cells contributes to asthma development. Conversely, exposure to high levels of LPS induces a Th17 cell response, leading to increased production of IL-17, which is associated with asthma, COPD, and lung cancer incidence. Responses to bacterial EV exposure can similarly be broadly divided based on whether one of two mechanisms, either intracellular or extracellular, is activated, which depends on the type of the parent cell. Extracellular bacteria-derived EVs can cause neutrophilic inflammation via Th17 cell induction, which is associated with asthma, emphysema, COPD, and lung cancer. On the other hand, intracellular bacteria-derived EVs lead to mononuclear inflammation via Th1 cell induction, which increases the risk of emphysema. In conclusion, future measures should focus on the overall reduction of LPS sources in addition to the improvement of the balance of inhaled bacterial EVs in the indoor environment to minimize pulmonary disease risk.
中文翻译:

细菌衍生的超细粉尘颗粒对肺部疾病的影响。
环境颗粒物暴露与健康之间的关系已经明确。已知直径为 100 nm 或更小的超细颗粒 (UFP) 会增加肺部疾病的风险。含有UFP的粉尘中的生物因素可引起严重的炎症反应。肺部疾病的发生主要是由于免疫功能障碍引起的慢性炎症的结果。因此,本综述重点关注室内灰尘中生物UFP(主要是脂多糖(LPS)和细菌细胞外囊泡(EV))对肺部的不利影响,以及与慢性肺部疾病发展有关的病理生理机制。 LPS 引起的肺部炎症的影响主要取决于吸入 LPS 的量。当吸入相对较低水平的 LPS 时,一系列免疫反应会导致 Th2 细胞诱导,而 Th2 细胞释放的 IL-5 和 IL-13 会导致哮喘的发生。相反,暴露于高水平的 LPS 会诱导 Th17 细胞反应,导致 IL-17 的产生增加,而 IL-17 与哮喘、慢性阻塞性肺病和肺癌的发病率有关。同样,对细菌 EV 暴露的反应可以根据细胞内或细胞外两种机制之一是否被激活来大致划分,这取决于亲代细胞的类型。细胞外细菌衍生的 EV 可通过 Th17 细胞诱导引起中性粒细胞炎症,这与哮喘、肺气肿、慢性阻塞性肺病和肺癌有关。另一方面,细胞内细菌衍生的 EV 通过 Th1 细胞诱导导致单核炎症,从而增加肺气肿的风险。 总之,未来的措施除了改善室内环境中吸入细菌EV的平衡外,还应重点关注整体减少LPS来源,以最大程度地降低肺部疾病风险。
更新日期:2020-04-24
中文翻译:

细菌衍生的超细粉尘颗粒对肺部疾病的影响。
环境颗粒物暴露与健康之间的关系已经明确。已知直径为 100 nm 或更小的超细颗粒 (UFP) 会增加肺部疾病的风险。含有UFP的粉尘中的生物因素可引起严重的炎症反应。肺部疾病的发生主要是由于免疫功能障碍引起的慢性炎症的结果。因此,本综述重点关注室内灰尘中生物UFP(主要是脂多糖(LPS)和细菌细胞外囊泡(EV))对肺部的不利影响,以及与慢性肺部疾病发展有关的病理生理机制。 LPS 引起的肺部炎症的影响主要取决于吸入 LPS 的量。当吸入相对较低水平的 LPS 时,一系列免疫反应会导致 Th2 细胞诱导,而 Th2 细胞释放的 IL-5 和 IL-13 会导致哮喘的发生。相反,暴露于高水平的 LPS 会诱导 Th17 细胞反应,导致 IL-17 的产生增加,而 IL-17 与哮喘、慢性阻塞性肺病和肺癌的发病率有关。同样,对细菌 EV 暴露的反应可以根据细胞内或细胞外两种机制之一是否被激活来大致划分,这取决于亲代细胞的类型。细胞外细菌衍生的 EV 可通过 Th17 细胞诱导引起中性粒细胞炎症,这与哮喘、肺气肿、慢性阻塞性肺病和肺癌有关。另一方面,细胞内细菌衍生的 EV 通过 Th1 细胞诱导导致单核炎症,从而增加肺气肿的风险。 总之,未来的措施除了改善室内环境中吸入细菌EV的平衡外,还应重点关注整体减少LPS来源,以最大程度地降低肺部疾病风险。











































 京公网安备 11010802027423号
京公网安备 11010802027423号