Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Association Between Surgical Approach and Major Surgical Complications in Patients Undergoing Total Hip Arthroplasty
JAMA ( IF 63.1 ) Pub Date : 2020-03-17 , DOI: 10.1001/jama.2020.0785 Daniel Pincus 1, 2, 3 , Richard Jenkinson 1, 2 , Michael Paterson 3 , Timothy Leroux 1, 4 , Bheeshma Ravi 1, 2, 3
JAMA ( IF 63.1 ) Pub Date : 2020-03-17 , DOI: 10.1001/jama.2020.0785 Daniel Pincus 1, 2, 3 , Richard Jenkinson 1, 2 , Michael Paterson 3 , Timothy Leroux 1, 4 , Bheeshma Ravi 1, 2, 3
Affiliation
|
Importance
Controversy exists about the preferred surgical approach for total hip arthroplasty (THA). Objective
To determine whether an anterior approach is associated with lower risk of complications than either a lateral or posterior approach. Design, Setting, and Participants
Population-based retrospective cohort study of all adults in Ontario, Canada, who had undergone primary THA for osteoarthritis between April 1, 2015, and March 31, 2018. All patients were followed up over a 1-year period (study end date, March 31, 2019). Exposures
Surgical approach (anterior vs lateral/posterior) for THA. Main Outcomes and Measures
Major surgical complications within 1 year (composite of deep infection requiring surgery, dislocation requiring closed or open reduction, or revision surgery). Outcomes were compared among propensity-score matched groups using Cox proportional hazards regression. Results
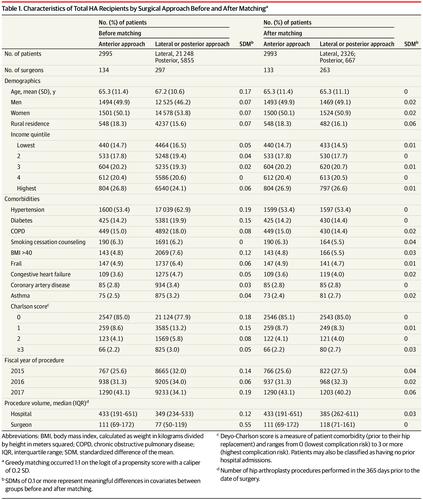
Of the 30 098 patients (mean [SD] age, 67 years [10.7 years]; 16 079 women [53.4%]) who underwent THA, 2995 (10%) underwent the anterior approach; 21 248 (70%), the lateral approach; and 5855 (20%) the posterior approach performed at 1 of 73 hospitals by 1 of 298 surgeons. All patients were followed up for 1 year. Compared with those undergoing the lateral or posterior approach, patients undergoing an anterior approach were younger (mean age, 65 vs 67 years; standardized difference, 0.17); had lower rates of morbid obesity (4.8% vs 7.6%; standardized difference, 0.12), diabetes (14.2% vs 19.9%; standardized difference, 0.15), and hypertension (53.4% vs 62.9%; standardized difference, 0.19); and were treated by higher-volume surgeons (median range, 111 procedures; interquartile range, 69-172 vs 77 procedures, interquartile range, 50-119 in the prior year; standardized difference, 0.55). Compared with 2993 propensity-score matched patients undergoing a lateral or posterior approach, the 2993 matched patients undergoing anterior approaches had a significantly greater risk of a major surgical complication (61 patients [2%] vs 29 patients [1%]; absolute risk difference, 1.07%; 95% CI, 0.46%-1.69%; hazard ratio, 2.07; 95% CI, 1.48 to 2.88). Conclusions and Relevance
Among patients undergoing total hip arthroplasty, an anterior surgical approach compared with a posterior or lateral surgical approach was associated with a small but statistically significant increased risk of major surgical complications. The findings may help inform decisions about surgical approach for hip arthroplasty, although further research is needed to understand pain and functional outcomes.
中文翻译:

全髋关节置换术患者手术入路与主要手术并发症的关系
重要性 关于全髋关节置换术 (THA) 的首选手术方法存在争议。目的 确定前入路是否与侧入路或后入路相比并发症风险更低。设计、设置和参与者 加拿大安大略省所有成年人在 2015 年 4 月 1 日至 2018 年 3 月 31 日期间因骨关节炎接受过初次 THA 的基于人群的回顾性队列研究。所有患者均接受了为期 1 年的随访(研究结束日期,2019 年 3 月 31 日)。暴露 THA 的手术入路(前侧 vs 侧侧/后侧)。主要结果和措施 1年内主要手术并发症(需要手术的深部感染,需要闭合或切开复位的脱位,或翻修手术)。使用 Cox 比例风险回归比较倾向评分匹配组之间的结果。结果 在接受 THA 的 30 098 名患者(平均 [SD] 年龄,67 岁 [10.7 岁];16 079 名女性 [53.4%])中,2995 名(10%)接受了前路入路;21 248 (70%),横向入路;298 名外科医生中的 1 名在 73 家医院中的 1 家进行了 5855 次(20%)后路手术。所有患者均获随访1年。与接受外侧入路或后入路的患者相比,接受前路入路的患者更年轻(平均年龄,65 vs 67 岁;标准化差异,0.17);病态肥胖率(4.8% 对 7.6%;标准化差为 0.12)、糖尿病(14.2% 对 19.9%;标准化差为 0.15)和高血压(53.4% 对 62.9%;标准化差为 0.19)的发生率较低;并由大手术量的外科医生进行治疗(中位数范围,111 次手术;四分位距,69-172 对 77 次手术,四分位距,前一年为 50-119;标准化差异,0.55)。与接受外侧入路或后入路的 2993 名倾向评分匹配的患者相比,接受前路入路的 2993 名匹配的患者发生主要手术并发症的风险显着更高(61 名患者 [2%] 对 29 名患者 [1%];绝对风险差异) ,1.07%;95% CI,0.46%-1.69%;风险比,2.07;95% CI,1.48 至 2.88)。结论和相关性 在接受全髋关节置换术的患者中,前路手术入路与后路或侧路手术入路相比,主要手术并发症的风险虽小但具有统计学意义。
更新日期:2020-03-17
中文翻译:

全髋关节置换术患者手术入路与主要手术并发症的关系
重要性 关于全髋关节置换术 (THA) 的首选手术方法存在争议。目的 确定前入路是否与侧入路或后入路相比并发症风险更低。设计、设置和参与者 加拿大安大略省所有成年人在 2015 年 4 月 1 日至 2018 年 3 月 31 日期间因骨关节炎接受过初次 THA 的基于人群的回顾性队列研究。所有患者均接受了为期 1 年的随访(研究结束日期,2019 年 3 月 31 日)。暴露 THA 的手术入路(前侧 vs 侧侧/后侧)。主要结果和措施 1年内主要手术并发症(需要手术的深部感染,需要闭合或切开复位的脱位,或翻修手术)。使用 Cox 比例风险回归比较倾向评分匹配组之间的结果。结果 在接受 THA 的 30 098 名患者(平均 [SD] 年龄,67 岁 [10.7 岁];16 079 名女性 [53.4%])中,2995 名(10%)接受了前路入路;21 248 (70%),横向入路;298 名外科医生中的 1 名在 73 家医院中的 1 家进行了 5855 次(20%)后路手术。所有患者均获随访1年。与接受外侧入路或后入路的患者相比,接受前路入路的患者更年轻(平均年龄,65 vs 67 岁;标准化差异,0.17);病态肥胖率(4.8% 对 7.6%;标准化差为 0.12)、糖尿病(14.2% 对 19.9%;标准化差为 0.15)和高血压(53.4% 对 62.9%;标准化差为 0.19)的发生率较低;并由大手术量的外科医生进行治疗(中位数范围,111 次手术;四分位距,69-172 对 77 次手术,四分位距,前一年为 50-119;标准化差异,0.55)。与接受外侧入路或后入路的 2993 名倾向评分匹配的患者相比,接受前路入路的 2993 名匹配的患者发生主要手术并发症的风险显着更高(61 名患者 [2%] 对 29 名患者 [1%];绝对风险差异) ,1.07%;95% CI,0.46%-1.69%;风险比,2.07;95% CI,1.48 至 2.88)。结论和相关性 在接受全髋关节置换术的患者中,前路手术入路与后路或侧路手术入路相比,主要手术并发症的风险虽小但具有统计学意义。











































 京公网安备 11010802027423号
京公网安备 11010802027423号