当前位置:
X-MOL 学术
›
J. Am. Coll. Cardiol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Oral Anticoagulation and Cardiovascular Outcomes in Patients With Atrial Fibrillation and End-Stage Renal Disease
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2020-03-01 , DOI: 10.1016/j.jacc.2020.01.019 Sean D. Pokorney , Eric Black-Maier , Anne S. Hellkamp , Daniel J. Friedman , Sreekanth Vemulapalli , Christopher B. Granger , Laine Thomas , Eric D. Peterson , Jonathan P. Piccini
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2020-03-01 , DOI: 10.1016/j.jacc.2020.01.019 Sean D. Pokorney , Eric Black-Maier , Anne S. Hellkamp , Daniel J. Friedman , Sreekanth Vemulapalli , Christopher B. Granger , Laine Thomas , Eric D. Peterson , Jonathan P. Piccini
|
BACKGROUND
Atrial fibrillation (AF) is common in patients with end-stage renal disease (ESRD). The impact of oral anticoagulation (OAC) in ESRD patients is uncertain. OBJECTIVES
The purpose of this study was to describe patterns of OAC use in ESRD patients with AF and their associations with cardiovascular outcomes. METHODS
Using Medicare fee-for-service 5% claims data from 2007 to 2013, we analyzed treatment and outcomes in a cohort of patients with ESRD and AF. Prescription drug benefit information was used to determine the timing of OAC therapy. Cox proportional hazards modeling was used to compare outcomes including death, all-cause stroke, ischemic stroke, hemorrhagic stroke, and bleeding hospitalizations in ESRD patients treated with or without OAC. RESULTS
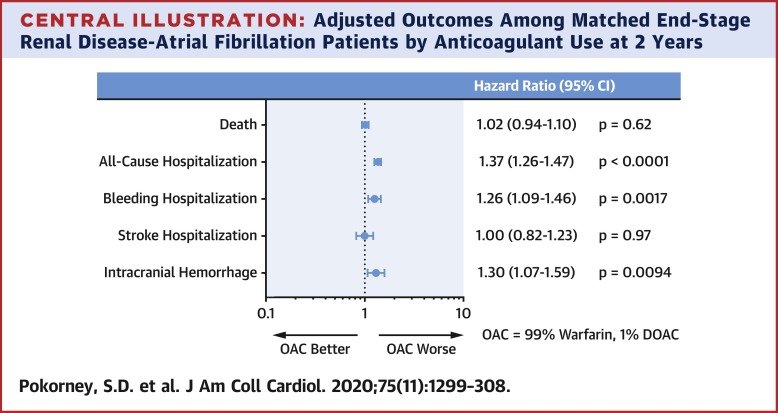
The cohort included 8,410 patients with AF and ESRD. A total of 3,043 (36.2%) patients were treated with OAC at some time during the study period. Propensity scores used to match 1,519 patients with AF and ESRD on OAC with 3,018 ESRD patients without OAC. Treatment with OAC was not associated with hospitalization for stroke (hazard ratio [HR]: 1.00; 95% confidence interval [CI]: 0.23 to 1.35; p = 0.97) or death (HR: 1.02; 95% CI: 0.94 to 1.10; p = 0.62). OAC was associated with an increased risk of hospitalization for bleeding (HR: 1.26; 95% CI: 1.09 to 1.46; p = 0.0017) and intracranial hemorrhage (HR: 1.30; 95% CI: 1.07 to 1.59; p = 0.0094). CONCLUSIONS
OAC utilization was low in patients with AF and ESRD. We found no association between OAC use and reduced risk of stroke or death. OAC use was associated with increased risks of hospitalization for bleeding or intracranial hemorrhage. Alternative stroke prevention strategies are needed in patients with ESRD and AF.
中文翻译:

心房颤动和终末期肾病患者的口服抗凝治疗和心血管结局
背景 心房颤动 (AF) 在终末期肾病 (ESRD) 患者中很常见。口服抗凝剂 (OAC) 对 ESRD 患者的影响尚不确定。目的 本研究的目的是描述 ESRD AF 患者使用 OAC 的模式及其与心血管结局的关系。方法 使用 2007 年至 2013 年的 Medicare 按服务收费 5% 索赔数据,我们分析了一组 ESRD 和 AF 患者的治疗和结果。处方药受益信息用于确定 OAC 治疗的时间。Cox 比例风险模型用于比较接受或不接受 OAC 治疗的 ESRD 患者的结局,包括死亡、全因卒中、缺血性卒中、出血性卒中和出血住院。结果 该队列包括 8,410 名 AF 和 ESRD 患者。共 3,043 (36. 2%) 患者在研究期间的某个时间接受了 OAC 治疗。倾向评分用于将 1,519 名使用 OAC 的 AF 和 ESRD 患者与 3,018 名未使用 OAC 的 ESRD 患者进行匹配。OAC 治疗与卒中住院(风险比 [HR]:1.00;95% 置信区间 [CI]:0.23 至 1.35;p = 0.97)或死亡(HR:1.02;95% CI:0.94 至 1.10; p = 0.62)。OAC 与出血住院风险增加有关(HR:1.26;95% CI:1.09 至 1.46;p = 0.0017)和颅内出血(HR:1.30;95% CI:1.07 至 1.59;p = 0.0094)。结论 AF 和 ESRD 患者的 OAC 利用率较低。我们发现使用 OAC 与降低中风或死亡风险之间没有关联。OAC 的使用与出血或颅内出血住院风险增加有关。
更新日期:2020-03-01
中文翻译:

心房颤动和终末期肾病患者的口服抗凝治疗和心血管结局
背景 心房颤动 (AF) 在终末期肾病 (ESRD) 患者中很常见。口服抗凝剂 (OAC) 对 ESRD 患者的影响尚不确定。目的 本研究的目的是描述 ESRD AF 患者使用 OAC 的模式及其与心血管结局的关系。方法 使用 2007 年至 2013 年的 Medicare 按服务收费 5% 索赔数据,我们分析了一组 ESRD 和 AF 患者的治疗和结果。处方药受益信息用于确定 OAC 治疗的时间。Cox 比例风险模型用于比较接受或不接受 OAC 治疗的 ESRD 患者的结局,包括死亡、全因卒中、缺血性卒中、出血性卒中和出血住院。结果 该队列包括 8,410 名 AF 和 ESRD 患者。共 3,043 (36. 2%) 患者在研究期间的某个时间接受了 OAC 治疗。倾向评分用于将 1,519 名使用 OAC 的 AF 和 ESRD 患者与 3,018 名未使用 OAC 的 ESRD 患者进行匹配。OAC 治疗与卒中住院(风险比 [HR]:1.00;95% 置信区间 [CI]:0.23 至 1.35;p = 0.97)或死亡(HR:1.02;95% CI:0.94 至 1.10; p = 0.62)。OAC 与出血住院风险增加有关(HR:1.26;95% CI:1.09 至 1.46;p = 0.0017)和颅内出血(HR:1.30;95% CI:1.07 至 1.59;p = 0.0094)。结论 AF 和 ESRD 患者的 OAC 利用率较低。我们发现使用 OAC 与降低中风或死亡风险之间没有关联。OAC 的使用与出血或颅内出血住院风险增加有关。











































 京公网安备 11010802027423号
京公网安备 11010802027423号