当前位置:
X-MOL 学术
›
Int. J. Obesity
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Impact of maternal obesity on placental transcriptome and morphology associated with fetal growth restriction in mice.
International Journal of Obesity ( IF 4.2 ) Pub Date : 2020-03-13 , DOI: 10.1038/s41366-020-0561-3 Daniela de Barros Mucci 1, 2, 3 , Laura C Kusinski 1 , Phoebe Wilsmore 1 , Elena Loche 1 , Lucas C Pantaleão 1 , Thomas J Ashmore 1 , Heather L Blackmore 1 , Denise S Fernandez-Twinn 1 , Maria das Graças T do Carmo 2 , Susan E Ozanne 1
International Journal of Obesity ( IF 4.2 ) Pub Date : 2020-03-13 , DOI: 10.1038/s41366-020-0561-3 Daniela de Barros Mucci 1, 2, 3 , Laura C Kusinski 1 , Phoebe Wilsmore 1 , Elena Loche 1 , Lucas C Pantaleão 1 , Thomas J Ashmore 1 , Heather L Blackmore 1 , Denise S Fernandez-Twinn 1 , Maria das Graças T do Carmo 2 , Susan E Ozanne 1
Affiliation
|
BACKGROUND
In utero exposure to obesity is consistently associated with increased risk of metabolic disease, obesity and cardiovascular dysfunction in later life despite the divergence of birth weight outcomes. The placenta plays a critical role in offspring development and long-term health, as it mediates the crosstalk between the maternal and fetal environments. However, its phenotypic and molecular modifications in the context of maternal obesity associated with fetal growth restriction (FGR) remain poorly understood.
METHODS
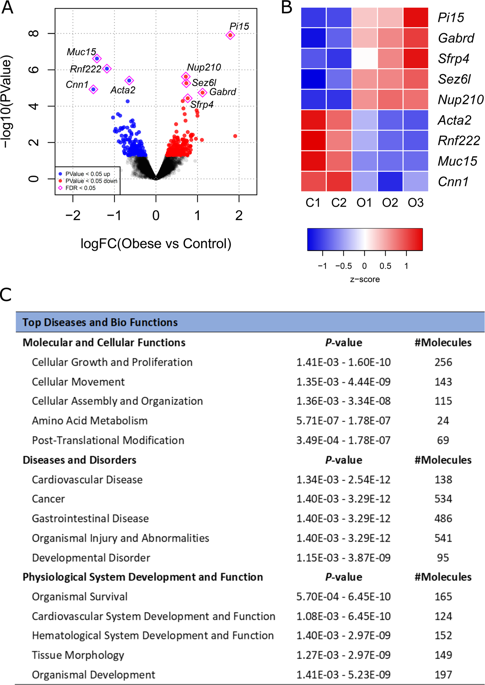
Using a mouse model of maternal diet-induced obesity, we investigated changes in the placental transcriptome through RNA sequencing (RNA-seq) and Ingenuity Pathway Analysis (IPA) at embryonic day (E) 19. The most differentially expressed genes (FDR < 0.05) were validated by Quantitative real-time PCR (qPCR) in male and female placentae at E19. The expression of these targets and related genes was also determined by qPCR at E13 to examine whether the observed alterations had an earlier onset at mid-gestation. Structural analyses were performed using immunofluorescent staining against Ki67 and CD31 to investigate phenotypic outcomes at both timepoints.
RESULTS
RNA-seq and IPA analyses revealed differential expression of transcripts and pathway interactions related to placental vascular development and tissue morphology in obese placentae at term, including downregulation of Muc15, Cnn1, and Acta2. Pdgfb, which is implicated in labyrinthine layer development, was downregulated in obese placentae at E13. This was consistent with the morphological evidence of reduced labyrinth zone (LZ) size, as well as lower fetal weight at both timepoints irrespective of offspring sex.
CONCLUSIONS
Maternal obesity results in abnormal placental LZ development and impaired vascularization, which may mediate the observed FGR through reduced transfer of nutrients across the placenta.
中文翻译:

母亲肥胖对与小鼠胎儿生长受限相关的胎盘转录组和形态的影响。
背景技术尽管出生体重结果存在差异,但在子宫内暴露于肥胖症始终与日后代谢疾病、肥胖症和心血管功能障碍的风险增加相关。胎盘在后代发育和长期健康中发挥着至关重要的作用,因为它介导母体和胎儿环境之间的串扰。然而,在与胎儿生长受限(FGR)相关的母亲肥胖背景下,其表型和分子修饰仍知之甚少。方法 使用母体饮食诱导肥胖的小鼠模型,通过 RNA 测序 (RNA-seq) 和独创性通路分析 (IPA) 在胚胎第 19 天 (E) 时研究胎盘转录组的变化。差异最大的基因 (FDR < 0。05) 通过定量实时 PCR (qPCR) 在 E19 的男性和女性胎盘中进行了验证。这些靶标和相关基因的表达也在 E13 时通过 qPCR 测定,以检查观察到的改变是否在妊娠中期较早发生。使用针对 Ki67 和 CD31 的免疫荧光染色进行结构分析,以研究两个时间点的表型结果。结果 RNA-seq 和 IPA 分析揭示了足月肥胖胎盘中与胎盘血管发育和组织形态相关的转录物和通路相互作用的差异表达,包括 Muc15、Cnn1 和 Acta2 的下调。Pdgfb 与迷路层发育有关,在 E13 时肥胖胎盘中表达下调。这与迷路区 (LZ) 尺寸减小的形态学证据一致,以及在两个时间点胎儿体重降低,无论后代性别如何。结论 孕妇肥胖会导致胎盘 LZ 发育异常和血管化受损,这可能通过减少营养物质通过胎盘的转移来介导观察到的 FGR。
更新日期:2020-04-24
中文翻译:

母亲肥胖对与小鼠胎儿生长受限相关的胎盘转录组和形态的影响。
背景技术尽管出生体重结果存在差异,但在子宫内暴露于肥胖症始终与日后代谢疾病、肥胖症和心血管功能障碍的风险增加相关。胎盘在后代发育和长期健康中发挥着至关重要的作用,因为它介导母体和胎儿环境之间的串扰。然而,在与胎儿生长受限(FGR)相关的母亲肥胖背景下,其表型和分子修饰仍知之甚少。方法 使用母体饮食诱导肥胖的小鼠模型,通过 RNA 测序 (RNA-seq) 和独创性通路分析 (IPA) 在胚胎第 19 天 (E) 时研究胎盘转录组的变化。差异最大的基因 (FDR < 0。05) 通过定量实时 PCR (qPCR) 在 E19 的男性和女性胎盘中进行了验证。这些靶标和相关基因的表达也在 E13 时通过 qPCR 测定,以检查观察到的改变是否在妊娠中期较早发生。使用针对 Ki67 和 CD31 的免疫荧光染色进行结构分析,以研究两个时间点的表型结果。结果 RNA-seq 和 IPA 分析揭示了足月肥胖胎盘中与胎盘血管发育和组织形态相关的转录物和通路相互作用的差异表达,包括 Muc15、Cnn1 和 Acta2 的下调。Pdgfb 与迷路层发育有关,在 E13 时肥胖胎盘中表达下调。这与迷路区 (LZ) 尺寸减小的形态学证据一致,以及在两个时间点胎儿体重降低,无论后代性别如何。结论 孕妇肥胖会导致胎盘 LZ 发育异常和血管化受损,这可能通过减少营养物质通过胎盘的转移来介导观察到的 FGR。











































 京公网安备 11010802027423号
京公网安备 11010802027423号