Journal of Allergy and Clinical Immunology ( IF 11.4 ) Pub Date : 2020-03-13 , DOI: 10.1016/j.jaci.2020.02.029 David G Mummy 1 , Katherine J Carey 2 , Michael D Evans 3 , Loren C Denlinger 4 , Mark L Schiebler 5 , Ronald L Sorkness 6 , Nizar N Jarjour 4 , Sean B Fain 7
|
Background
There is an unmet need for an objective biomarker to predict asthma exacerbations.
Objective
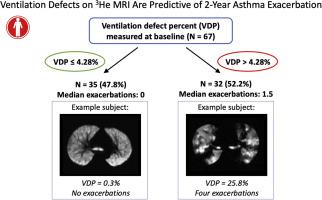
Our aim was to assess the ventilation defect percent (VDP) on hyperpolarized helium-3 magnetic resonance imaging as a predictor of exacerbation frequency following imaging.
Methods
Subjects underwent hyperpolarized helium-3 and conventional clinical measurements, including pulmonary function tests, during a period of disease stability, and exacerbations were recorded prospectively over the following 2 years. We used a Poisson regression tree model to estimate an optimal VDP threshold for classifying subjects into high- versus low-exacerbation groups and then used statistical regression to compare this VDP threshold against conventional clinical measures as predictors of exacerbations.
Results
A total of 67 individuals with asthma (27 males and 40 females, 28 with mild-to-moderate asthma and 39 with severe asthma) had a median VDP of 3.75% (1.2% [first quartile]-7.9% [third quartile]). An optimal VDP threshold of 4.28% was selected on the basis of the maximum likelihood estimation of the regression tree model. Subjects with a VDP greater than 4.28% (n = 32) had a median of 1.5 exacerbations versus 0.0 for subjects with a VDP less than 4.28% (n = 35). In a stepwise multivariate regression model, a VDP greater than 4.28% was associated with an exacerbation incidence rate ratio of 2.5 (95% CI = 1.3-4.7) versus a VDP less than or equal to 4.28%. However, once individual medical history was included in the model, VDP was no longer significant. Nonetheless, VDP may provide an objective and complementary quantitative marker of individual exacerbation risk that is useful for monitoring individual change in disease status, selecting patients for therapy, and assessing treatment response.
Conclusion
VDP measured with magnetic resonance imaging shows promise as a biomarker of prospective asthma exacerbations.
中文翻译:

哮喘患者超极化氦 3 MRI 的通气缺陷可预测 2 年恶化频率。
背景
对预测哮喘恶化的客观生物标志物的需求尚未得到满足。
客观的
我们的目的是评估超极化氦 3 磁共振成像的通气缺陷百分比 (VDP),作为成像后恶化频率的预测指标。
方法
受试者在疾病稳定期间接受超极化氦 3 和常规临床测量,包括肺功能测试,并在接下来的 2 年内前瞻性地记录恶化。我们使用泊松回归树模型来估计最佳 VDP 阈值,用于将受试者分为高恶化组和低恶化组,然后使用统计回归将这个 VDP 阈值与作为恶化预测因子的常规临床措施进行比较。
结果
共有 67 名哮喘患者(27 名男性和 40 名女性,28 名轻中度哮喘患者和 39 名重度哮喘患者)的中位 VDP 为 3.75%(1.2% [第一四分位数]-7.9% [第三四分位数]) . 在回归树模型的最大似然估计的基础上,选择了 4.28% 的最佳 VDP 阈值。VDP 大于 4.28% (n = 32) 的受试者的恶化中位数为 1.5,而 VDP 小于 4.28% (n = 35) 的受试者为 0.0。在逐步多元回归模型中,大于 4.28% 的 VDP 与 2.5(95% CI = 1.3-4.7)的加重发生率比值与小于或等于 4.28% 的 VDP 相关。然而,一旦模型中包含个人病史,VDP 就不再重要。尽管如此,
结论
用磁共振成像测量的 VDP 显示出作为前瞻性哮喘恶化的生物标志物的前景。











































 京公网安备 11010802027423号
京公网安备 11010802027423号