PLOS Medicine ( IF 10.5 ) Pub Date : 2020-03-12 , DOI: 10.1371/journal.pmed.1003048 Hatem A Wafa 1, 2, 3 , Charles D A Wolfe 1, 2, 3 , Ajay Bhalla 1, 4 , Yanzhong Wang 1, 2, 3
|
Background
There have been reductions in stroke mortality over recent decades, but estimates by aetiological subtypes are limited. This study estimates time trends in mortality and functional dependence by ischaemic stroke (IS) aetiological subtype over a 16-year period.
Methods and findings
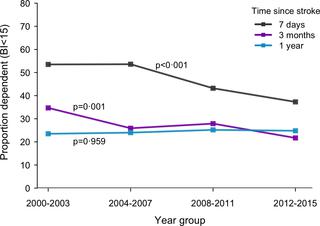
The study population was 357,308 in 2011; 50.4% were males, 56% were white, and 25% were of black ethnic backgrounds. Population-based case ascertainment of stroke was conducted, and all participants who had their first-ever IS between 2000 and 2015 were identified. Further classification was concluded according to the underlying mechanism into large-artery atherosclerosis (LAA), cardio-embolism (CE), small-vessel occlusion (SVO), other determined aetiologies (OTH), and undetermined aetiologies (UND). Temporal trends in survival rates were examined using proportional-hazards survival modelling, adjusted for demography, prestroke risk factors, case mix variables, and processes of care. We carried out additional regression analyses to explore patterns in case-fatality rates (CFRs) at 30 days and 1 year and to explore whether these trends occurred at the expense of greater functional dependence (Barthel Index [BI] < 15) among survivors. A total of 3,128 patients with first-ever ISs were registered. The median age was 70.7 years; 50.9% were males; and 66.2% were white, 25.5% were black, and 8.3% were of other ethnic groups. Between 2000–2003 and 2012–2015, the adjusted overall mortality decreased by 24% (hazard ratio [HR] per year 0.976; 95% confidence interval [CI] 0.959–0.993). Mortality reductions were equally noted in both sexes and in the white and black populations but were only significant in CE strokes (HR per year 0.972; 95% CI 0.945‒0.998) and in patients aged ≥55 years (HR per year 0.975; 95% CI 0.959‒0.992). CFRs within 30 days and 1 year after an IS declined by 38% (rate ratio [RR] per year 0.962; 95% CI 0.941‒0.984) and 37% (RR per year 0.963; 95% CI 0.949‒0.976), respectively. Recent IS was independently associated with a 23% reduced risk of functional dependence at 3 months after onset (RR per year 0.983; 95% CI 0.968–0.998; p = 0.002 for trend). The study is limited by small number of events in certain subgroups (e.g., LAA), which could have led to insufficient power to detect significant trends.
Conclusions
Both mortality and 3-month functional dependence after IS decreased by an annual average of around 2.4% and 1.7%, respectively, during 2000‒2015. Such reductions were particularly evident in strokes of CE origins and in those aged ≥55 years.
中文翻译:

缺血性中风后死亡和依赖性的长期趋势:一项使用南伦敦中风登记册(SLSR)的回顾性队列研究。
背景
近几十年来,中风死亡率有所降低,但按病因亚型进行的估计有限。这项研究估算了16年间缺血性卒中(IS)病因亚型的死亡率和功能依赖性的时间趋势。
方法和发现
2011年的研究人口为357,308;男性占50.4%,白人占56%,黑人背景占25%。进行了基于人群的中风病例确定,并鉴定了所有在2000年至2015年间首次出现IS的参与者。根据潜在机制将进一步的分类归纳为大动脉粥样硬化(LAA),心脏栓塞(CE),小血管闭塞(SVO),其他确定的病因(OTH)和不确定的病因(UND)。使用比例风险生存模型检查生存率的时间趋势,并根据人口统计学,中风前危险因素,病例混合变量和护理过程进行调整。我们进行了额外的回归分析,以探讨30天和1年时的病死率(CFR)的模式,并探讨这些趋势是否以幸存者中更大的功能依赖性为代价(Barthel Index [BI] <15)发生。总共登记了3,128例首次有IS的患者。中位年龄是70.7岁。男性占50.9%;白人占66.2%,黑人占25.5%,其他族裔占8.3%。在2000–2003年至2012–2015年之间,调整后的总死亡率下降了24%(每年的危险比[HR]为0.976; 95%的置信区间[CI]为0.959-0.993)。男女,白人和黑人的死亡率均降低,但仅在CE卒中(每年HR 0.972; 95%CI 0.945‒0.998)和≥55岁患者(每年HR 0.975; 95%)中显着降低CI 0.959‒0.992)。IS发生后30天和1年内的CFR分别下降了38%(每年比率[RR] 0.962; 95%CI 0.941‒0.984)和37%(每年RR 0.963; 95%CI 0.949‒0.976)。发作后3个月,近期IS与功能依赖风险降低23%独立相关(每年RR 0.983; 95%CI 0.968-0.998;p = 0.002(趋势)。该研究受到某些亚组(例如,LAA)中少量事件的限制,这可能导致不足以检测重大趋势。
结论
在2000-2015年间,IS后的死亡率和3个月的功能依赖性分别年均下降约2.4%和1.7%。这种减少在CE起源的卒中和≥55岁的人群中尤为明显。











































 京公网安备 11010802027423号
京公网安备 11010802027423号