当前位置:
X-MOL 学术
›
Cancer Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Differences in physician opinions about controversial issues surrounding contralateral prophylactic mastectomy (CPM): A survey of physicians from accredited breast centers in the United States.
Cancer Medicine ( IF 2.9 ) Pub Date : 2020-03-11 , DOI: 10.1002/cam4.2914 Katharine Yao 1 , Richard Bleicher 2 , Meena Moran 3 , Cecilia Chang 4 , Jill Dietz 5 , Vered Stearns 6 , James Connolly 7 , Terry Sarantou 8 , Scott Kurtzman 9 ,
Cancer Medicine ( IF 2.9 ) Pub Date : 2020-03-11 , DOI: 10.1002/cam4.2914 Katharine Yao 1 , Richard Bleicher 2 , Meena Moran 3 , Cecilia Chang 4 , Jill Dietz 5 , Vered Stearns 6 , James Connolly 7 , Terry Sarantou 8 , Scott Kurtzman 9 ,
Affiliation
|
BACKGROUND
Indications and insurance coverage for contralateral prophylactic mastectomy (CPM) and CPM as a quality measure are controversial. Few studies have examined physician opinions on these issues.
METHODS
A cross-sectional survey of multi-specialty physicians at the National Accreditation Program for Breast Centers from 2017-2018 examined opinions on insurance coverage for CPM, CPM as a quality measure, and indications for CPM. A multivariate logistic regression was used to assess physician and facility factors associated with likelihood to recommend CPM.
RESULTS
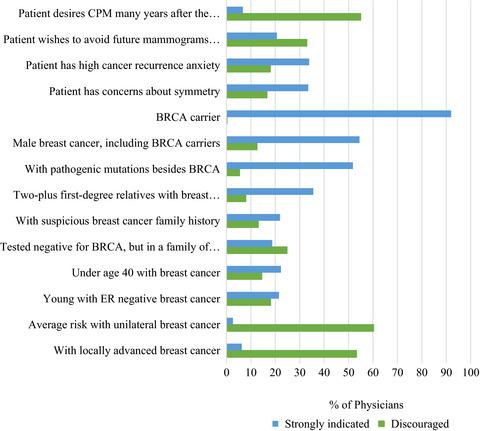
Of 2412 physicians, 1226 responded from 382 facilities for a physician response rate of 50.8%. There were 300 (24.5%) medical oncologists, 316 (25.8%) radiation oncologists, 248 (20.2%) plastic surgeons, and 322 (26.3%) oncologic or general surgeons. Three hundred and ninety-eight (37%) physicians favor insurance coverage for all patients and 520 (46.6%) for patients at average CBC risk. Four hundred and fifty (40%) of all physicians felt physician specific rates of CPM should be a hospital quality measure. BRCA deleterious mutation carrier status was the most common indication to recommend CPM (n = 1043; 92%) and 684 (60.2%) physicians discourage CPM for average contralateral risk (CBC) patients. After adjusting for physician and facility factors, the only significant predictor of higher likelihood to recommend CPM for average CBC risk patients were plastics surgeons (OR = 8.3 (95%CI 2.4-29.1)) P = .0009).
CONCLUSION
There is consensus among physicians on the most appropriate indication for CPM but opinions vary on CPM as a quality measure and insurance coverage for CPM. These findings can help guide discussions on CPM among a multidisciplinary team of physicians.
中文翻译:

医生对围绕对侧预防性乳房切除术 (CPM) 的有争议问题的意见分歧:对美国经认可的乳房中心的医生的调查。
背景 对侧预防性乳房切除术 (CPM) 和 CPM 作为质量衡量指标的适应症和保险范围存在争议。很少有研究检查医生对这些问题的看法。方法 对 2017 年至 2018 年国家乳腺中心认证计划的多专科医师进行的横断面调查研究了关于 CPM 保险范围、作为质量衡量标准的 CPM 以及 CPM 适应症的意见。多变量逻辑回归用于评估与推荐 CPM 的可能性相关的医生和设施因素。结果 在 2412 名医生中,有 1226 名来自 382 家机构,医生回应率为 50.8%。有 300 (24.5%) 名肿瘤内科医生、316 (25.8%) 名放射肿瘤科医生、248 (20.2%) 名整形外科医生和 322 (26.3%) 名肿瘤或普通外科医生。398 (37%) 名医生赞成为所有患者提供保险,520 (46.6%) 名医生赞成为平均 CBC 风险的患者提供保险。四百五十 (40%) 的所有医生认为医生特定的 CPM 率应该是医院质量的衡量标准。BRCA 有害突变携带者状态是推荐 CPM 的最常见指征(n = 1043;92%),684(60.2%)名医生不鼓励对平均对侧风险 (CBC) 患者进行 CPM。在调整医生和设施因素后,为平均 CBC 风险患者推荐 CPM 的唯一重要预测因素是整形外科医生 (OR = 8.3 (95%CI 2.4-29.1)) P = .0009)。结论 对于 CPM 最合适的适应症,医生们达成了共识,但对 CPM 作为 CPM 的质量衡量标准和保险范围的看法各不相同。
更新日期:2020-03-11
中文翻译:

医生对围绕对侧预防性乳房切除术 (CPM) 的有争议问题的意见分歧:对美国经认可的乳房中心的医生的调查。
背景 对侧预防性乳房切除术 (CPM) 和 CPM 作为质量衡量指标的适应症和保险范围存在争议。很少有研究检查医生对这些问题的看法。方法 对 2017 年至 2018 年国家乳腺中心认证计划的多专科医师进行的横断面调查研究了关于 CPM 保险范围、作为质量衡量标准的 CPM 以及 CPM 适应症的意见。多变量逻辑回归用于评估与推荐 CPM 的可能性相关的医生和设施因素。结果 在 2412 名医生中,有 1226 名来自 382 家机构,医生回应率为 50.8%。有 300 (24.5%) 名肿瘤内科医生、316 (25.8%) 名放射肿瘤科医生、248 (20.2%) 名整形外科医生和 322 (26.3%) 名肿瘤或普通外科医生。398 (37%) 名医生赞成为所有患者提供保险,520 (46.6%) 名医生赞成为平均 CBC 风险的患者提供保险。四百五十 (40%) 的所有医生认为医生特定的 CPM 率应该是医院质量的衡量标准。BRCA 有害突变携带者状态是推荐 CPM 的最常见指征(n = 1043;92%),684(60.2%)名医生不鼓励对平均对侧风险 (CBC) 患者进行 CPM。在调整医生和设施因素后,为平均 CBC 风险患者推荐 CPM 的唯一重要预测因素是整形外科医生 (OR = 8.3 (95%CI 2.4-29.1)) P = .0009)。结论 对于 CPM 最合适的适应症,医生们达成了共识,但对 CPM 作为 CPM 的质量衡量标准和保险范围的看法各不相同。









































 京公网安备 11010802027423号
京公网安备 11010802027423号