当前位置:
X-MOL 学术
›
Br. J. Cancer
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
An integrated analysis of lymphocytic reaction, tumour molecular characteristics and patient survival in colorectal cancer.
British Journal of Cancer ( IF 8.8 ) Pub Date : 2020-03-11 , DOI: 10.1038/s41416-020-0780-3 Koichiro Haruki 1 , Keisuke Kosumi 1 , Peilong Li 2 , Kota Arima 1 , Juha P Väyrynen 1, 3 , Mai Chan Lau 1 , Tyler S Twombly 1 , Tsuyoshi Hamada 1 , Jonathan N Glickman 4 , Kenji Fujiyoshi 1 , Yang Chen 1 , Chunxia Du 1 , Chunguang Guo 1 , Sara A Väyrynen 5 , Andressa Dias Costa 5 , Mingyang Song 6, 7, 8 , Andrew T Chan 7, 8, 9, 10 , Jeffrey A Meyerhardt 5 , Reiko Nishihara 1, 6, 11, 12 , Charles S Fuchs 13, 14, 15 , Li Liu 1, 6, 16 , Xuehong Zhang 9 , Kana Wu 6, 9, 11 , Marios Giannakis 5, 17, 18 , Jonathan A Nowak 1 , Shuji Ogino 1, 11, 17, 19
British Journal of Cancer ( IF 8.8 ) Pub Date : 2020-03-11 , DOI: 10.1038/s41416-020-0780-3 Koichiro Haruki 1 , Keisuke Kosumi 1 , Peilong Li 2 , Kota Arima 1 , Juha P Väyrynen 1, 3 , Mai Chan Lau 1 , Tyler S Twombly 1 , Tsuyoshi Hamada 1 , Jonathan N Glickman 4 , Kenji Fujiyoshi 1 , Yang Chen 1 , Chunxia Du 1 , Chunguang Guo 1 , Sara A Väyrynen 5 , Andressa Dias Costa 5 , Mingyang Song 6, 7, 8 , Andrew T Chan 7, 8, 9, 10 , Jeffrey A Meyerhardt 5 , Reiko Nishihara 1, 6, 11, 12 , Charles S Fuchs 13, 14, 15 , Li Liu 1, 6, 16 , Xuehong Zhang 9 , Kana Wu 6, 9, 11 , Marios Giannakis 5, 17, 18 , Jonathan A Nowak 1 , Shuji Ogino 1, 11, 17, 19
Affiliation
|
BACKGROUND
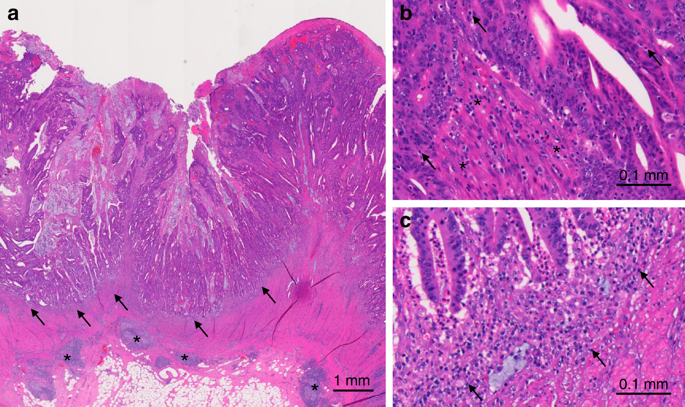
Histological lymphocytic reaction is regarded as an independent prognostic marker in colorectal cancer. Considering the lack of adequate statistical power, adjustment for selection bias and comprehensive tumour molecular data in most previous studies, we investigated the strengths of the prognostic associations of lymphocytic reaction in colorectal carcinoma by utilising an integrative database of two prospective cohort studies.
METHODS
We examined Crohn's-like reaction, intratumoural periglandular reaction, peritumoural reaction and tumour-infiltrating lymphocytes in 1465 colorectal carcinoma cases. Using covariate data of 4420 colorectal cancer cases in total, inverse probability-weighted Cox proportional hazard regression model was used to control for selection bias (due to tissue availability) and potential confounders, including stage, MSI status, LINE-1 methylation, PTGS2 and CTNNB1 expression, KRAS, BRAF and PIK3CA mutations, and tumour neoantigen load.
RESULTS
Higher levels of each lymphocytic reaction component were associated with better colorectal cancer-specific survival (Ptrend < 0.002). Compared with cases with negative/low intratumoural periglandular reaction, multivariable-adjusted HRs were 0.55 (95% CI, 0.42-0.71) in cases with intermediate reaction and 0.20 (95% CI, 0.12-0.35) in cases with high reaction. These relationships were consistent in strata of MSI status or neoantigen loads (Pinteraction > 0.2).
CONCLUSIONS
The four lymphocytic reaction components are prognostic biomarkers in colorectal carcinoma.
中文翻译:

结直肠癌淋巴细胞反应、肿瘤分子特征和患者生存的综合分析。
背景技术组织学淋巴细胞反应被认为是结直肠癌的独立预后标志物。考虑到在大多数先前的研究中缺乏足够的统计能力、对选择偏倚的调整和全面的肿瘤分子数据,我们利用两个前瞻性队列研究的综合数据库研究了结直肠癌中淋巴细胞反应的预后关联的强度。方法我们检查了1465例结直肠癌病例的克罗恩样反应、瘤内腺周反应、瘤周反应和肿瘤浸润淋巴细胞。使用总共 4420 例结直肠癌病例的协变量数据,使用逆概率加权 Cox 比例风险回归模型来控制选择偏差(由于组织可用性)和潜在的混杂因素,包括分期、MSI 状态、LINE-1 甲基化、PTGS2 和 CTNNB1 表达、KRAS、BRAF 和 PIK3CA 突变以及肿瘤新抗原负荷。结果 每种淋巴细胞反应成分的较高水平与较好的结直肠癌特异性生存率相关(Ptrend < 0.002)。与肿瘤内腺周反应阴性/低的病例相比,多变量调整的HRs在中等反应病例中为0.55(95% CI,0.42-0.71),在高反应病例中为0.20(95% CI,0.12-0.35)。这些关系在 MSI 状态或新抗原负荷的分层中是一致的 (Pinteraction > 0.2)。结论 四种淋巴细胞反应成分是结直肠癌的预后生物标志物。结果 每种淋巴细胞反应成分的较高水平与较好的结直肠癌特异性生存率相关(Ptrend < 0.002)。与肿瘤内腺周反应阴性/低的病例相比,多变量调整的HRs在中等反应病例中为0.55(95% CI,0.42-0.71),在高反应病例中为0.20(95% CI,0.12-0.35)。这些关系在 MSI 状态或新抗原负荷的分层中是一致的 (Pinteraction > 0.2)。结论 四种淋巴细胞反应成分是结直肠癌的预后生物标志物。结果 每种淋巴细胞反应成分的较高水平与较好的结直肠癌特异性生存率相关(Ptrend < 0.002)。与肿瘤内腺周反应阴性/低的病例相比,多变量调整的HRs在中等反应病例中为0.55(95% CI,0.42-0.71),在高反应病例中为0.20(95% CI,0.12-0.35)。这些关系在 MSI 状态或新抗原负荷的分层中是一致的 (Pinteraction > 0.2)。结论 四种淋巴细胞反应成分是结直肠癌的预后生物标志物。71) 在中等反应的情况下和 0.20 (95% CI, 0.12-0.35) 在高反应的情况下。这些关系在 MSI 状态或新抗原负荷的分层中是一致的 (Pinteraction > 0.2)。结论 四种淋巴细胞反应成分是结直肠癌的预后生物标志物。71) 在中等反应的情况下和 0.20 (95% CI, 0.12-0.35) 在高反应的情况下。这些关系在 MSI 状态或新抗原负荷的分层中是一致的 (Pinteraction > 0.2)。结论 四种淋巴细胞反应成分是结直肠癌的预后生物标志物。
更新日期:2020-03-12
中文翻译:

结直肠癌淋巴细胞反应、肿瘤分子特征和患者生存的综合分析。
背景技术组织学淋巴细胞反应被认为是结直肠癌的独立预后标志物。考虑到在大多数先前的研究中缺乏足够的统计能力、对选择偏倚的调整和全面的肿瘤分子数据,我们利用两个前瞻性队列研究的综合数据库研究了结直肠癌中淋巴细胞反应的预后关联的强度。方法我们检查了1465例结直肠癌病例的克罗恩样反应、瘤内腺周反应、瘤周反应和肿瘤浸润淋巴细胞。使用总共 4420 例结直肠癌病例的协变量数据,使用逆概率加权 Cox 比例风险回归模型来控制选择偏差(由于组织可用性)和潜在的混杂因素,包括分期、MSI 状态、LINE-1 甲基化、PTGS2 和 CTNNB1 表达、KRAS、BRAF 和 PIK3CA 突变以及肿瘤新抗原负荷。结果 每种淋巴细胞反应成分的较高水平与较好的结直肠癌特异性生存率相关(Ptrend < 0.002)。与肿瘤内腺周反应阴性/低的病例相比,多变量调整的HRs在中等反应病例中为0.55(95% CI,0.42-0.71),在高反应病例中为0.20(95% CI,0.12-0.35)。这些关系在 MSI 状态或新抗原负荷的分层中是一致的 (Pinteraction > 0.2)。结论 四种淋巴细胞反应成分是结直肠癌的预后生物标志物。结果 每种淋巴细胞反应成分的较高水平与较好的结直肠癌特异性生存率相关(Ptrend < 0.002)。与肿瘤内腺周反应阴性/低的病例相比,多变量调整的HRs在中等反应病例中为0.55(95% CI,0.42-0.71),在高反应病例中为0.20(95% CI,0.12-0.35)。这些关系在 MSI 状态或新抗原负荷的分层中是一致的 (Pinteraction > 0.2)。结论 四种淋巴细胞反应成分是结直肠癌的预后生物标志物。结果 每种淋巴细胞反应成分的较高水平与较好的结直肠癌特异性生存率相关(Ptrend < 0.002)。与肿瘤内腺周反应阴性/低的病例相比,多变量调整的HRs在中等反应病例中为0.55(95% CI,0.42-0.71),在高反应病例中为0.20(95% CI,0.12-0.35)。这些关系在 MSI 状态或新抗原负荷的分层中是一致的 (Pinteraction > 0.2)。结论 四种淋巴细胞反应成分是结直肠癌的预后生物标志物。71) 在中等反应的情况下和 0.20 (95% CI, 0.12-0.35) 在高反应的情况下。这些关系在 MSI 状态或新抗原负荷的分层中是一致的 (Pinteraction > 0.2)。结论 四种淋巴细胞反应成分是结直肠癌的预后生物标志物。71) 在中等反应的情况下和 0.20 (95% CI, 0.12-0.35) 在高反应的情况下。这些关系在 MSI 状态或新抗原负荷的分层中是一致的 (Pinteraction > 0.2)。结论 四种淋巴细胞反应成分是结直肠癌的预后生物标志物。



























 京公网安备 11010802027423号
京公网安备 11010802027423号