JACC: Cardiovascular Interventions ( IF 11.7 ) Pub Date : 2020-03-11 , DOI: 10.1016/j.jcin.2019.11.018 Ariel Roguin , Rosaly A. Buiten , Carine J.M. Doggen , Ofer Kobo , Paolo Zocca , Peter W. Danse , Carl E. Schotborgh , Gillian A.J. Jessurun , K. Gert van Houwelingen , Martin G. Stoel , R. Melvyn Tjon Joe Gin , Gerard C.M. Linssen , Clemens von Birgelen
|
Objectives
This study sought to assess 2-year clinical outcome following percutaneous coronary intervention (PCI) with thin-strut new-generation drug-eluting stents (DES) in patients treated in proximal left anterior descending artery (P-LAD) versus non–P-LAD lesions.
Background
In current revascularization guidelines, P-LAD coronary artery stenosis is discussed separately, mainly because of a higher adverse event risk and benefits of bypass surgery.
Methods
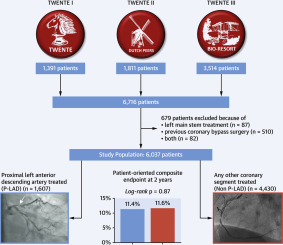
The study included 6,037 patients without previous bypass surgery or left main stem involvement from the TWENTE I, II, and III randomized trials. A total of 1,607 (26.6%) patients had at least 1 DES implanted in P-LAD and were compared with 4,430 (73.4%) patients who were exclusively treated in other (non–P-LAD) segments.
Results
Two-year follow-up was available in 5,995 (99.3%) patients. At baseline, P-LAD patients had more multivessel treatment and longer total stent length. The rate of the patient-oriented composite clinical endpoint (any death, any myocardial infarction, or any revascularization) was similar in P-LAD versus non–P-LAD patients (11.4% vs. 11.6%; p = 0.87). In P-LAD patients, the rate of the device-oriented composite clinical endpoint (cardiac death, target vessel myocardial infarction, or target lesion revascularization) was higher (7.6% vs. 6.0%; p = 0.020), driven by a higher rate of target vessel myocardial infarction (4.1% vs. 2.6%; p = 0.002). However, multivariate analysis showed no independent association between stenting P-LAD lesions and clinical endpoints.
Conclusions
In this patient-level pooled analysis of 3 large-scale contemporary DES trials, treatment of P-LAD lesions was not independently associated with higher 2-year adverse clinical event rates. These results imply that separate consideration in future revascularization guidelines may not be mandatory any longer.
中文翻译:

薄支撑新一代药物洗脱支架治疗近端LAD
目标
这项研究旨在评估使用左前降支近端动脉(P-LAD)与非P-冠状动脉治疗的新一代细支气管新生药物洗脱支架(DES)经皮冠状动脉介入治疗(PCI)后的2年临床疗效。 LAD病变。
背景
在当前的血运重建指南中,单独讨论了P-LAD冠状动脉狭窄,主要是因为较高的不良事件风险和旁路手术的益处。
方法
该研究纳入了6037例先前未进行旁路手术或左主干受累的TWENTE I,II和III随机试验的患者。共有1607名患者(26.6%)至少有1位DES植入了P-LAD中,而仅在其他(非P-LAD)部分中接受治疗的患者则有4,430名(73.4%)。
结果
5,995(99.3%)位患者可以进行两年的随访。基线时,P-LAD患者接受更多的多支血管治疗,支架总长度更长。以患者为导向的复合临床终点(任何死亡,任何心肌梗塞或任何血运重建)的发生率在P-LAD患者与非P-LAD患者中相似(11.4%对11.6%; p = 0.87)。在P-LAD患者中,设备导向型复合临床终点(心脏死亡,靶血管心肌梗塞或靶病变血运重建)的发生率较高(7.6%vs. 6.0%; p = 0.020),这是由较高的发生率引起的目标血管心肌梗塞的发生率(4.1%vs. 2.6%; p = 0.002)。但是,多变量分析显示支架置入P-LAD病变与临床终点之间无独立关联。
结论
在这项对3项当代大型DES试验进行的患者水平汇总分析中,P-LAD病变的治疗与2年不良临床事件发生率较高无关。这些结果表明,将来的血运重建指南中的单独考虑可能不再是强制性的。











































 京公网安备 11010802027423号
京公网安备 11010802027423号