当前位置:
X-MOL 学术
›
J. Am. Coll. Cardiol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Nonculprit Lesion Myocardial Infarction Following Percutaneous Coronary Intervention in Patients With Acute Coronary Syndrome
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2020-03-01 , DOI: 10.1016/j.jacc.2019.12.067 Benjamin M. Scirica , Brian A. Bergmark , David A. Morrow , Elliott M. Antman , Marc P. Bonaca , Sabina A. Murphy , Marc S. Sabatine , Eugene Braunwald , Stephen D. Wiviott
Journal of the American College of Cardiology ( IF 21.7 ) Pub Date : 2020-03-01 , DOI: 10.1016/j.jacc.2019.12.067 Benjamin M. Scirica , Brian A. Bergmark , David A. Morrow , Elliott M. Antman , Marc P. Bonaca , Sabina A. Murphy , Marc S. Sabatine , Eugene Braunwald , Stephen D. Wiviott
|
BACKGROUND
Recent emphasis on reduced duration and/or intensity of antiplatelet therapy following percutaneous coronary intervention (PCI) irrespective of indication for PCI may fail to account for the substantial risk of subsequent nontarget lesion events in acute coronary syndrome (ACS) patients. OBJECTIVES
The authors sought to examine the effect of more potent antiplatelet therapy on the basis of the timing and etiology of recurrent myocardial infarction (MI) or cardiovascular death following PCI for ACS. METHODS
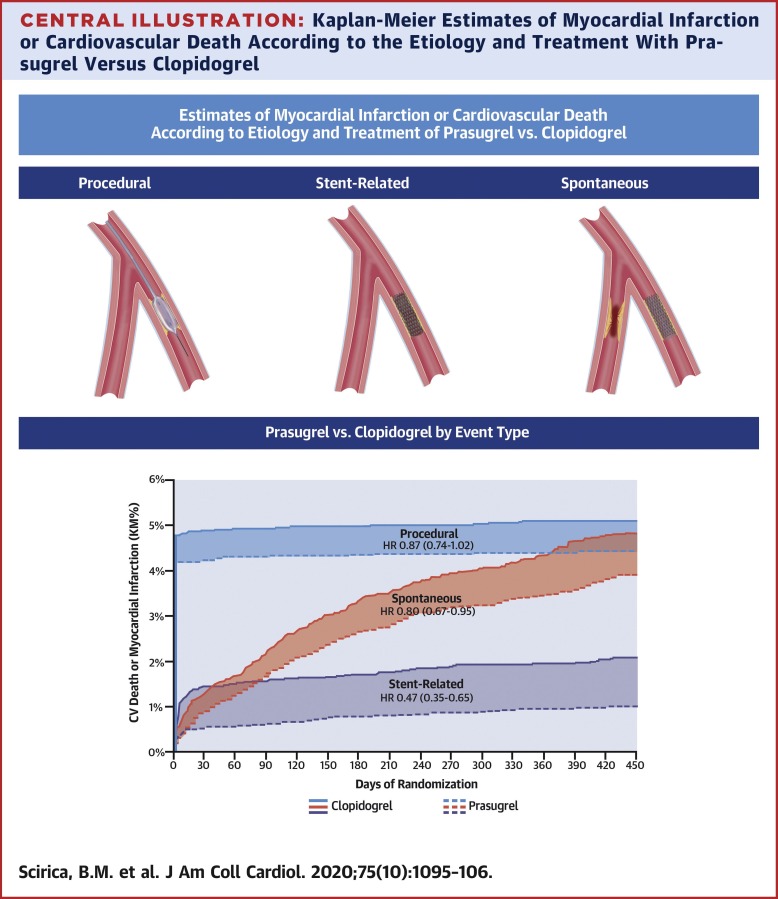
In the TRITON-TIMI 38 study (Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition With Prasugrel-Thrombolysis In Myocardial Infarction 38), which randomized patients to prasugrel or clopidogrel, 12,844 patients with ACS received at least 1 stent. MI and cardiovascular death were categorized as: 1) procedural (related to revascularization); 2) definite or probable stent thrombosis (ST); or 3) spontaneous (non-ST or non-procedure-related). Median follow-up was 14.5 months. RESULTS
Among the first events occurring within 30 days, 584 (69.0%) were procedural, 126 (14.9%) ST-related, and 136 (16.1%) spontaneous. After 30 days, 22 (4.7%) were procedural, 63 (13.5%) were ST-related, and 383 (81.8%) spontaneous. Prasugrel significantly reduced the incidence of MI or cardiovascular death for ST-related (1.0% vs. 2.1%; p < 0.001) and spontaneous events (3.9% vs. 4.8%; p = 0.012), with a directionally consistent numerical reduction for procedural events (4.4% vs. 5.1%; p = 0.078). Prasugrel increased spontaneous, but not procedural, major bleeding. CONCLUSIONS
Long-term potent antithrombotic therapy reduces de novo (spontaneous) atherothrombotic events in addition to preventing complications associated with stenting of the culprit lesion following ACS. In patients undergoing PCI for ACS, spontaneous events predominate after 30 days, with the later-phase cardiovascular benefit of potent dual antiplatelet therapy driven largely by reducing de novo atherothrombotic ischemic events. (Comparison of Prasugrel [CS-747] and Clopidogrel in Acute Coronary Syndrome Subjects Who Are to Undergo Percutaneous Coronary Intervention; NCT00097591).
中文翻译:

急性冠状动脉综合征患者经皮冠状动脉介入治疗后非罪犯病变心肌梗死
背景 最近强调在经皮冠状动脉介入治疗 (PCI) 后减少抗血小板治疗的持续时间和/或强度,而不管 PCI 的适应症如何,可能无法解释急性冠状动脉综合征 (ACS) 患者随后发生非靶病变事件的重大风险。目标作者试图根据 ACS 的 PCI 后复发性心肌梗死 (MI) 或心血管死亡的时间和病因来检查更有效的抗血小板治疗的效果。方法 在 TRITON-TIMI 38 研究(通过在心肌梗塞中使用普拉格雷溶栓治疗优化血小板抑制来评估治疗结果改善的试验 38)中,将患者随机分配至普拉格雷或氯吡格雷组,12,844 名 ACS 患者至少接受了 1 个支架。MI和心血管死亡被分类为:1) 程序性的(与血运重建相关);2) 明确或可能的支架内血栓形成 (ST);或 3) 自发的(非 ST 或非程序相关的)。中位随访时间为 14.5 个月。结果 在 30 天内发生的首次事件中,584 起 (69.0%) 是程序性的,126 起 (14.9%) 与 ST 相关,136 起 (16.1%) 是自发性的。30 天后,22 例 (4.7%) 是程序性的,63 例 (13.5%) 是 ST 相关的,383 例 (81.8%) 是自发性的。普拉格雷显着降低了 ST 相关(1.0% 对 2.1%;p < 0.001)和自发事件(3.9% 对 4.8%;p = 0.012)的 MI 或心血管死亡发生率,并在方向上一致地降低了程序性事件(4.4% 对 5.1%;p = 0.078)。普拉格雷增加了自发性而非程序性的大出血。结论 长期有效的抗血栓治疗可减少新发(自发性)动脉粥样硬化血栓形成事件,此外还可以预防 ACS 后与罪犯病变支架置入术相关的并发症。在因 ACS 接受 PCI 的患者中,自发事件在 30 天后占主导地位,强效双重抗血小板治疗的后期心血管益处主要是由减少新发动脉粥样硬化血栓形成的缺血事件驱动的。(普拉格雷 [CS-747] 和氯吡格雷在接受经皮冠状动脉介入治疗的急性冠状动脉综合征受试者中的比较;NCT00097591)。强效双重抗血小板治疗的后期心血管益处主要是由减少新发动脉粥样硬化血栓形成的缺血事件驱动的。(普拉格雷 [CS-747] 和氯吡格雷在接受经皮冠状动脉介入治疗的急性冠状动脉综合征受试者中的比较;NCT00097591)。强效双重抗血小板治疗的后期心血管益处主要是由减少新发动脉粥样硬化血栓形成的缺血事件驱动的。(普拉格雷 [CS-747] 和氯吡格雷在接受经皮冠状动脉介入治疗的急性冠状动脉综合征受试者中的比较;NCT00097591)。
更新日期:2020-03-01
中文翻译:

急性冠状动脉综合征患者经皮冠状动脉介入治疗后非罪犯病变心肌梗死
背景 最近强调在经皮冠状动脉介入治疗 (PCI) 后减少抗血小板治疗的持续时间和/或强度,而不管 PCI 的适应症如何,可能无法解释急性冠状动脉综合征 (ACS) 患者随后发生非靶病变事件的重大风险。目标作者试图根据 ACS 的 PCI 后复发性心肌梗死 (MI) 或心血管死亡的时间和病因来检查更有效的抗血小板治疗的效果。方法 在 TRITON-TIMI 38 研究(通过在心肌梗塞中使用普拉格雷溶栓治疗优化血小板抑制来评估治疗结果改善的试验 38)中,将患者随机分配至普拉格雷或氯吡格雷组,12,844 名 ACS 患者至少接受了 1 个支架。MI和心血管死亡被分类为:1) 程序性的(与血运重建相关);2) 明确或可能的支架内血栓形成 (ST);或 3) 自发的(非 ST 或非程序相关的)。中位随访时间为 14.5 个月。结果 在 30 天内发生的首次事件中,584 起 (69.0%) 是程序性的,126 起 (14.9%) 与 ST 相关,136 起 (16.1%) 是自发性的。30 天后,22 例 (4.7%) 是程序性的,63 例 (13.5%) 是 ST 相关的,383 例 (81.8%) 是自发性的。普拉格雷显着降低了 ST 相关(1.0% 对 2.1%;p < 0.001)和自发事件(3.9% 对 4.8%;p = 0.012)的 MI 或心血管死亡发生率,并在方向上一致地降低了程序性事件(4.4% 对 5.1%;p = 0.078)。普拉格雷增加了自发性而非程序性的大出血。结论 长期有效的抗血栓治疗可减少新发(自发性)动脉粥样硬化血栓形成事件,此外还可以预防 ACS 后与罪犯病变支架置入术相关的并发症。在因 ACS 接受 PCI 的患者中,自发事件在 30 天后占主导地位,强效双重抗血小板治疗的后期心血管益处主要是由减少新发动脉粥样硬化血栓形成的缺血事件驱动的。(普拉格雷 [CS-747] 和氯吡格雷在接受经皮冠状动脉介入治疗的急性冠状动脉综合征受试者中的比较;NCT00097591)。强效双重抗血小板治疗的后期心血管益处主要是由减少新发动脉粥样硬化血栓形成的缺血事件驱动的。(普拉格雷 [CS-747] 和氯吡格雷在接受经皮冠状动脉介入治疗的急性冠状动脉综合征受试者中的比较;NCT00097591)。强效双重抗血小板治疗的后期心血管益处主要是由减少新发动脉粥样硬化血栓形成的缺血事件驱动的。(普拉格雷 [CS-747] 和氯吡格雷在接受经皮冠状动脉介入治疗的急性冠状动脉综合征受试者中的比较;NCT00097591)。











































 京公网安备 11010802027423号
京公网安备 11010802027423号