Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Prevalence of polypoidal choroidal vasculopathy in Caucasian patients as estimated from optical coherence tomography signs
Eye ( IF 2.8 ) Pub Date : 2020-03-09 , DOI: 10.1038/s41433-020-0834-z Gerald Liew 1, 2 , Helen Do Hyun-Jin 2, 3 , Claire Hooper 2 , Ee-Mun Chia 2 , Paul Mitchell 1 , Stephen Ong 2 , I-Van Ho 2, 3
Eye ( IF 2.8 ) Pub Date : 2020-03-09 , DOI: 10.1038/s41433-020-0834-z Gerald Liew 1, 2 , Helen Do Hyun-Jin 2, 3 , Claire Hooper 2 , Ee-Mun Chia 2 , Paul Mitchell 1 , Stephen Ong 2 , I-Van Ho 2, 3
Affiliation
|
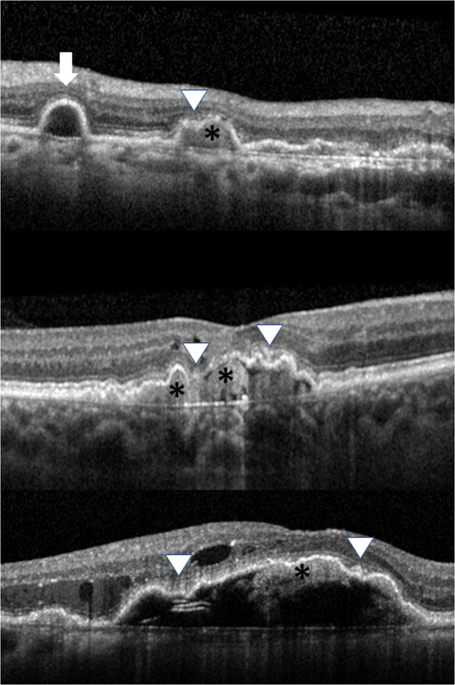
Polypoidal choroidal vasculopathy (PCV) is increasingly recognised as an important cause of choroidal neovascularisation. PCV is characterised by the presence of large choroidal polyps with an associated branching vascular network. These lesions are distinct from the more diffuse choroidal neovascularisation in neovascular macular degeneration (nAMD). PCV has traditionally been thought to be rare in Caucasian patients, with prevalence estimates of 7.2–10.3% in clinic populations presenting with nAMD [1]. However, there is increasing evidence PCV that may be underrecognized in Caucasian patients, as studies that have specifically looked for PCV in Caucasian patients report much higher prevalence of up to 32% [2]. ICGA is the gold standard for diagnosing PCV but is impractical to perform in all patients due to the cost, risk of adverse reactions, and need for specialised equipment. Recently our group and others have reported spectral domain optical coherence tomography (SD-OCT) can be used to diagnose PCV with high accuracy [3, 4]. A combination of at least three out of four SD-OCT features (peaked retinal pigment epithelium detachment (PED), multiple PEDs, PED notch, hyperreflective material within the PED, Fig. 1) has high sensitivity (95%) and specificity (93-95%) for diagnosing PCV [3, 4]. We conducted a retrospective clinic-based cohort study to determine the prevalence of PCV in Caucasian patients. A masked grader extracted and reviewed SD-OCT scans, fundus fluorescein angiograms, ICG angiograms, and medical records of consecutive patients who underwent anti-VEGF treatment for nAMD at a tertiary referral retinal practice in Sydney, Australia, from January 2017 to June 2019. Inclusion criteria were treatment-naïve patients, a documented diagnosis of nAMD or PCV by the treating retinal specialist, and SD-OCT of gradable quality prior to starting anti-VEGF therapy. Initial SD-OCT scans were reviewed for the presence of the four OCT features described above. If three or four out of four signs were identified, the eye was classified as having OCT diagnosed PCV. The prevalence was compared with that of eyes having ICGA diagnosed PCV. ICGA was only performed to confirm the diagnosis in eyes that had a high clinical suspicion of having PCV, based on clinical features such as orange polyps on clinical examination, moderate or severe retinal haemorrhage, or a notched haemorrhage. The study was approved by the Human Research Ethics Committee of the University of Sydney, Sydney, Australia. A total of 90 patients (100 eyes) were identified meeting inclusion criteria. At initial presentation, 8 out of 100 eyes had ICGA diagnosed PCV (8%). Based on SD-OCT criteria, 22 (22%) of eyes were further categorised as having OCT diagnosed PCV, including all eight confirmed on ICGA. These patients were slightly younger than those with nAMD (77.6 ± 8.6 years vs. 81.0 ± 9.3 years) with slight male predominance (47.1 vs. 34.3%) but these differences were not statistically significant (p > 0.05). Our results add to accumulating evidence that PCV may be underdiagnosed in Caucasian populations [2]. Underlying PCV rather than nAMD may be a major reason why some eyes do not respond well to anti-VEGF therapy alone, as suggested by a recent study showing 50% of nonresponsive eyes had PCV as diagnosed on ICGA [2]. Such patients may benefit from either switching VEGF agents [5] or combination treatment with photodynamic therapy [6]. Our results suggest that PCV is likely under recognised in Caucasian populations by up to twofold or more, and that careful analysis of SD-OCT changes can help to detect this. * Gerald Liew gerald.liew@sydney.edu.au
中文翻译:

根据光学相干断层扫描体征估计白种人患者息肉状脉络膜血管病变的患病率
息肉状脉络膜血管病(PCV)越来越被认为是脉络膜新生血管形成的重要原因。PCV 的特点是存在大的脉络膜息肉和相关的分支血管网络。这些病变与新生血管性黄斑变性 (nAMD) 中更弥散的脉络膜新生血管不同。传统上认为 PCV 在白种人患者中很少见,临床人群中的 nAMD 患病率估计为 7.2-10.3% [1]。然而,越来越多的证据表明高加索患者可能未充分认识到 PCV,因为专门在高加索患者中寻找 PCV 的研究报告称其患病率要高得多,高达 32% [2]。ICGA 是诊断 PCV 的金标准,但由于成本、不良反应风险、并且需要专门的设备。最近我们小组和其他人报告了光谱域光学相干断层扫描 (SD-OCT) 可用于高精度诊断 PCV [3, 4]。四个 SD-OCT 特征中至少三个的组合(峰值视网膜色素上皮脱离 (PED)、多个 PED、PED 缺口、PED 内的高反射材料,图 1)具有高灵敏度 (95%) 和特异性 (93 -95%) 用于诊断 PCV [3, 4]。我们进行了一项基于临床的回顾性队列研究,以确定高加索患者中 PCV 的患病率。一名蒙面分级员提取并审查了 2017 年 1 月至 2019 年 6 月在澳大利亚悉尼的三级转诊视网膜实践中接受抗 VEGF 治疗 nAMD 的连续患者的 SD-OCT 扫描、眼底荧光素血管造影、ICG 血管造影和医疗记录。纳入标准是未接受过治疗的患者、经治疗的视网膜专家对 nAMD 或 PCV 的记录诊断,以及在开始抗 VEGF 治疗之前具有可分级质量的 SD-OCT。检查初始 SD-OCT 扫描是否存在上述四个 OCT 特征。如果确定了四个体征中的三个或四个,则将眼睛分类为 OCT 诊断为 PCV。将患病率与 ICGA 诊断为 PCV 的眼睛的患病率进行比较。ICGA 仅用于根据临床特征(如临床检查中的橙色息肉、中度或重度视网膜出血或切口出血)对临床高度怀疑患有 PCV 的眼睛进行诊断。该研究得到了澳大利亚悉尼大学人类研究伦理委员会的批准。共有 90 名患者(100 只眼)被确定符合纳入标准。初次就诊时,100 只眼中有 8 只眼经 ICGA 诊断为 PCV(8%)。根据 SD-OCT 标准,22 只(22%)的眼睛被进一步归类为 OCT 诊断为 PCV,包括在 ICGA 上确认的所有 8 只眼睛。这些患者比 nAMD 患者稍年轻(77.6 ± 8.6 岁 vs. 81.0 ± 9.3 岁),男性略占优势(47.1 vs. 34.3%),但这些差异无统计学意义(p > 0.05)。我们的结果增加了越来越多的证据表明,PCV 在白种人人群中可能被漏诊 [2]。潜在的 PCV 而不是 nAMD 可能是一些眼睛对单独的抗 VEGF 治疗反应不佳的主要原因,正如最近的一项研究表明,50% 的无反应眼睛在 ICGA 上诊断为 PCV [2]。此类患者可能受益于转换 VEGF 药物 [5] 或与光动力疗法联合治疗 [6]。我们的结果表明,PCV 在高加索人群中的识别率可能高达两倍或更多,对 SD-OCT 变化的仔细分析有助于发现这一点。* 杰拉尔德·刘 gerald.liew@sydney.edu.au
更新日期:2020-03-09
中文翻译:

根据光学相干断层扫描体征估计白种人患者息肉状脉络膜血管病变的患病率
息肉状脉络膜血管病(PCV)越来越被认为是脉络膜新生血管形成的重要原因。PCV 的特点是存在大的脉络膜息肉和相关的分支血管网络。这些病变与新生血管性黄斑变性 (nAMD) 中更弥散的脉络膜新生血管不同。传统上认为 PCV 在白种人患者中很少见,临床人群中的 nAMD 患病率估计为 7.2-10.3% [1]。然而,越来越多的证据表明高加索患者可能未充分认识到 PCV,因为专门在高加索患者中寻找 PCV 的研究报告称其患病率要高得多,高达 32% [2]。ICGA 是诊断 PCV 的金标准,但由于成本、不良反应风险、并且需要专门的设备。最近我们小组和其他人报告了光谱域光学相干断层扫描 (SD-OCT) 可用于高精度诊断 PCV [3, 4]。四个 SD-OCT 特征中至少三个的组合(峰值视网膜色素上皮脱离 (PED)、多个 PED、PED 缺口、PED 内的高反射材料,图 1)具有高灵敏度 (95%) 和特异性 (93 -95%) 用于诊断 PCV [3, 4]。我们进行了一项基于临床的回顾性队列研究,以确定高加索患者中 PCV 的患病率。一名蒙面分级员提取并审查了 2017 年 1 月至 2019 年 6 月在澳大利亚悉尼的三级转诊视网膜实践中接受抗 VEGF 治疗 nAMD 的连续患者的 SD-OCT 扫描、眼底荧光素血管造影、ICG 血管造影和医疗记录。纳入标准是未接受过治疗的患者、经治疗的视网膜专家对 nAMD 或 PCV 的记录诊断,以及在开始抗 VEGF 治疗之前具有可分级质量的 SD-OCT。检查初始 SD-OCT 扫描是否存在上述四个 OCT 特征。如果确定了四个体征中的三个或四个,则将眼睛分类为 OCT 诊断为 PCV。将患病率与 ICGA 诊断为 PCV 的眼睛的患病率进行比较。ICGA 仅用于根据临床特征(如临床检查中的橙色息肉、中度或重度视网膜出血或切口出血)对临床高度怀疑患有 PCV 的眼睛进行诊断。该研究得到了澳大利亚悉尼大学人类研究伦理委员会的批准。共有 90 名患者(100 只眼)被确定符合纳入标准。初次就诊时,100 只眼中有 8 只眼经 ICGA 诊断为 PCV(8%)。根据 SD-OCT 标准,22 只(22%)的眼睛被进一步归类为 OCT 诊断为 PCV,包括在 ICGA 上确认的所有 8 只眼睛。这些患者比 nAMD 患者稍年轻(77.6 ± 8.6 岁 vs. 81.0 ± 9.3 岁),男性略占优势(47.1 vs. 34.3%),但这些差异无统计学意义(p > 0.05)。我们的结果增加了越来越多的证据表明,PCV 在白种人人群中可能被漏诊 [2]。潜在的 PCV 而不是 nAMD 可能是一些眼睛对单独的抗 VEGF 治疗反应不佳的主要原因,正如最近的一项研究表明,50% 的无反应眼睛在 ICGA 上诊断为 PCV [2]。此类患者可能受益于转换 VEGF 药物 [5] 或与光动力疗法联合治疗 [6]。我们的结果表明,PCV 在高加索人群中的识别率可能高达两倍或更多,对 SD-OCT 变化的仔细分析有助于发现这一点。* 杰拉尔德·刘 gerald.liew@sydney.edu.au









































 京公网安备 11010802027423号
京公网安备 11010802027423号