当前位置:
X-MOL 学术
›
J. Hepatol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Portopulmonary hypertension in the current era of pulmonary hypertension management
Journal of Hepatology ( IF 25.7 ) Pub Date : 2020-07-01 , DOI: 10.1016/j.jhep.2020.02.021 Laurent Savale 1 , Manuel Guimas 2 , Nathan Ebstein 3 , Marie Fertin 4 , Mitja Jevnikar 1 , Sébastien Renard 5 , Delphine Horeau-Langlard 6 , Cécile Tromeur 7 , Céline Chabanne 8 , Grégoire Prevot 9 , Ari Chaouat 10 , Pamela Moceri 11 , Élise Artaud-Macari 12 , Bruno Degano 13 , Romain Tresorier 14 , Clément Boissin 15 , Hélène Bouvaist 16 , Anne-Claire Simon 17 , Marianne Riou 18 , Nicolas Favrolt 19 , Sylvain Palat 20 , Delphine Bourlier 21 , Pascal Magro 22 , Vincent Cottin 23 , Emmanuel Bergot 2 , Nicolas Lamblin 4 , Xavier Jaïs 1 , Audrey Coilly 24 , François Durand 25 , Claire Francoz 25 , Filomena Conti 26 , Philippe Hervé 1 , Gérald Simonneau 1 , David Montani 1 , Jean-Charles Duclos-Vallée 24 , Didier Samuel 24 , Marc Humbert 1 , Pascal De Groote 4 , Olivier Sitbon 1
Journal of Hepatology ( IF 25.7 ) Pub Date : 2020-07-01 , DOI: 10.1016/j.jhep.2020.02.021 Laurent Savale 1 , Manuel Guimas 2 , Nathan Ebstein 3 , Marie Fertin 4 , Mitja Jevnikar 1 , Sébastien Renard 5 , Delphine Horeau-Langlard 6 , Cécile Tromeur 7 , Céline Chabanne 8 , Grégoire Prevot 9 , Ari Chaouat 10 , Pamela Moceri 11 , Élise Artaud-Macari 12 , Bruno Degano 13 , Romain Tresorier 14 , Clément Boissin 15 , Hélène Bouvaist 16 , Anne-Claire Simon 17 , Marianne Riou 18 , Nicolas Favrolt 19 , Sylvain Palat 20 , Delphine Bourlier 21 , Pascal Magro 22 , Vincent Cottin 23 , Emmanuel Bergot 2 , Nicolas Lamblin 4 , Xavier Jaïs 1 , Audrey Coilly 24 , François Durand 25 , Claire Francoz 25 , Filomena Conti 26 , Philippe Hervé 1 , Gérald Simonneau 1 , David Montani 1 , Jean-Charles Duclos-Vallée 24 , Didier Samuel 24 , Marc Humbert 1 , Pascal De Groote 4 , Olivier Sitbon 1
Affiliation
|
BACKGROUND & AIMS
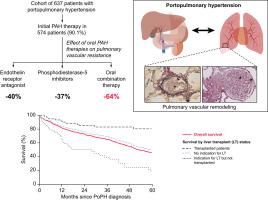
Long-term outcomes in portopulmonary hypertension (PoPH) are poorly studied in the current management era of pulmonary hypertension. We analysed the effect of pulmonary arterial hypertension (PAH)-targeted therapies, the survival and the predictors of death in a large contemporary cohort of patients with PoPH. METHODS
Data from patients with PoPH consecutively enrolled in the French Pulmonary Hypertension Registry between 2007 and 2017 were collected. Effect of initial treatment strategies on functional class, exercise capacity and cardiopulmonary haemodynamics were analysed. Survival and its association with PAH- and hepatic-related characteristics were also examined. RESULTS
Six hundred and thirty-seven patients (mean age 55±10 years; 58% male) were included. Fifty seven percent had mild cirrhosis, i.e. Child-Pugh (CP) stage A. The median MELD score was 11 (Q1-Q3; 9-15). Most patients (n=474; 74%) were initiated on monotherapy, either with a phosphodiesterase-5 inhibitor (n=336) or with an endothelin-receptor antagonist (n=128); 95 (15%) were initiated on double oral combination therapy and 5 (1%) on triple therapy. After a median treatment time of 4.5 months, there were significant improvements in functional class (p<0.001), 6-minute walk distance (6MWD) (p<0.0001) and pulmonary vascular resistance (p<0.0001). Overall survival rates were 84%, 69% and 51% at 1, 3 and 5 years, respectively. Baseline 6MWD, sex, age and MELD Score or CP stage were identified as independent prognostic factors. Survival from PoPH diagnosis was significantly better in the subgroup of patients who underwent liver transplantation (92%, 83% and 81% at 1, 3 and 5 years, respectively) CONCLUSION: Survival of patients with PoPH is strongly associated with the severity of liver disease. Patients who underwent liver transplantation had the best long-term outcomes.
中文翻译:

当前肺动脉高压管理时代的门静脉高压
背景和目的 在当前的肺动脉高压管理时代,门静脉高压 (PoPH) 的长期结果研究很少。我们在一个大型当代 PoPH 患者队列中分析了肺动脉高压 (PAH) 靶向治疗的效果、生存率和死亡预测因素。方法 收集了 2007 年至 2017 年连续入组法国肺动脉高压登记处的 PoPH 患者的数据。分析了初始治疗策略对功能等级、运动能力和心肺血流动力学的影响。还检查了存活率及其与 PAH 和肝脏相关特征的关联。结果 包括 637 名患者(平均年龄 55±10 岁;58% 为男性)。57% 有轻度肝硬化,即 Child-Pugh (CP) A 阶段。 MELD 评分中位数为 11(Q1-Q3;9-15)。大多数患者(n=474;74%)开始单药治疗,使用磷酸二酯酶 5 抑制剂(n=336)或内皮素受体拮抗剂(n=128);95 人 (15%) 开始接受双重口服联合治疗,5 人 (1%) 接受三联疗法。中位治疗时间为 4.5 个月后,功能等级 (p<0.001)、6 分钟步行距离 (6MWD) (p<0.0001) 和肺血管阻力 (p<0.0001) 均有显着改善。1、3 和 5 年的总生存率分别为 84%、69% 和 51%。基线 6MWD、性别、年龄和 MELD 评分或 CP 分期被确定为独立的预后因素。在接受肝移植的患者亚组中,PoPH 诊断的存活率显着提高(1 时分别为 92%、83% 和 81%,3 年和 5 年) 结论:PoPH 患者的存活率与肝病的严重程度密切相关。接受肝移植的患者的长期预后最好。
更新日期:2020-07-01
中文翻译:

当前肺动脉高压管理时代的门静脉高压
背景和目的 在当前的肺动脉高压管理时代,门静脉高压 (PoPH) 的长期结果研究很少。我们在一个大型当代 PoPH 患者队列中分析了肺动脉高压 (PAH) 靶向治疗的效果、生存率和死亡预测因素。方法 收集了 2007 年至 2017 年连续入组法国肺动脉高压登记处的 PoPH 患者的数据。分析了初始治疗策略对功能等级、运动能力和心肺血流动力学的影响。还检查了存活率及其与 PAH 和肝脏相关特征的关联。结果 包括 637 名患者(平均年龄 55±10 岁;58% 为男性)。57% 有轻度肝硬化,即 Child-Pugh (CP) A 阶段。 MELD 评分中位数为 11(Q1-Q3;9-15)。大多数患者(n=474;74%)开始单药治疗,使用磷酸二酯酶 5 抑制剂(n=336)或内皮素受体拮抗剂(n=128);95 人 (15%) 开始接受双重口服联合治疗,5 人 (1%) 接受三联疗法。中位治疗时间为 4.5 个月后,功能等级 (p<0.001)、6 分钟步行距离 (6MWD) (p<0.0001) 和肺血管阻力 (p<0.0001) 均有显着改善。1、3 和 5 年的总生存率分别为 84%、69% 和 51%。基线 6MWD、性别、年龄和 MELD 评分或 CP 分期被确定为独立的预后因素。在接受肝移植的患者亚组中,PoPH 诊断的存活率显着提高(1 时分别为 92%、83% 和 81%,3 年和 5 年) 结论:PoPH 患者的存活率与肝病的严重程度密切相关。接受肝移植的患者的长期预后最好。



























 京公网安备 11010802027423号
京公网安备 11010802027423号