Cell Death Discovery ( IF 6.1 ) Pub Date : 2020-03-04 , DOI: 10.1038/s41420-020-0245-8 Gaku Tsuji 1, 2 , Akiko Hashimoto-Hachiya 2 , Vu Hai Yen 2 , Masaki Takemura 2 , Ayako Yumine 1 , Kazuhisa Furue 2 , Masutaka Furue 1, 2, 3 , Takeshi Nakahara 2, 3
|
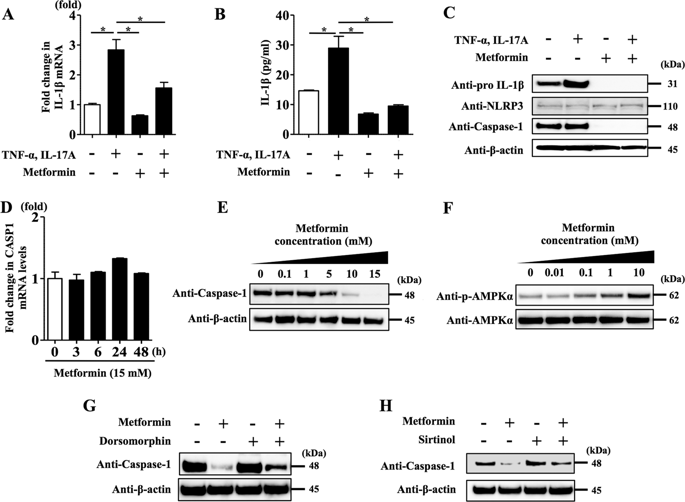
Psoriasis is a systemic inflammatory disease significantly associated with comorbidities including type 2 diabetes mellitus (T2DM). Metformin is utilized as a first-line agent for treating T2DM. Although metformin reportedly inhibits mature IL-1β secretion via NLRP3 inflammasome in macrophages of T2DM patients, it remains unclear whether it affects skin inflammation in psoriasis. To test this, we analysed normal human epidermal keratinocytes (NHEKs), a major skin component, stimulated with the key mediators of psoriasis development, TNF-α and IL-17A. This stimulation induced the upregulation of pro-IL-1β mRNA and protein levels, and subsequently mature IL-1β secretion, which was inhibited by metformin treatment. To further reveal the mechanism involved, we examined how metformin treatment affected NLRP3 inflammasome activated by TNF-α and IL-17A stimulation. We found that this treatment downregulated caspase-1 expression, a key mediator of NLRP3 inflammasome. Furthermore, inhibitors of AMPK and SIRT1 abrogated the downregulation of caspase-1 induced by metformin treatment, indicating that AMPK and SIRT1 are essential for the inhibitory effect on NLRP3 inflammasome in NHEKs. As IL-1β stimulation induced upregulation of IL-36γ, CXCL1, CXCL2, CCL20, S100A7, S100A8 and S100A9 mRNA and protein levels in NHEKs, we examined whether metformin treatment affects such gene expression. Metformin treatment inhibited upregulation of IL-36γ, CXCL1, CXCL2, CCL20, S100A7, S100A8 and S100A9 mRNA and protein levels induced by TNF-α and IL-17A stimulation. Finally, we examined whether metformin administration affected psoriasis development in an imiquimod-induced mouse psoriasis model. Oral metformin treatment significantly decreased ear thickness, epidermal hyperplasia and inflammatory cell infiltration. A cytokine profile in the epidermis under metformin treatment showed that IL-1β, Cxcl1, Cxcl2, S100a7, S100a8 and S100A9 mRNA levels were downregulated compared with control levels. These results indicate that metformin administration prevented psoriasis development in vivo. Collectively, our findings suggest that metformin-mediated anti-psoriatic effects on the skin have the potential for treating psoriasis in T2DM patients.
中文翻译:

二甲双胍通过损害角质形成细胞中的 NLRP3 炎性体来抑制 IL-1β 分泌:对预防银屑病发展的影响
银屑病是一种全身性炎症性疾病,与 2 型糖尿病 (T2DM) 等合并症显着相关。二甲双胍被用作治疗 T2DM 的一线药物。尽管据报道二甲双胍通过 NLRP3 炎症小体抑制 T2DM 患者巨噬细胞中成熟 IL-1β 的分泌,但尚不清楚它是否影响银屑病的皮肤炎症。为了测试这一点,我们分析了正常人表皮角质形成细胞 (NHEK),这是一种主要的皮肤成分,受到牛皮癣发展的关键介质 TNF-α 和 IL-17A 的刺激。这种刺激诱导 IL-1β 前体 mRNA 和蛋白质水平上调,随后导致成熟的 IL-1β 分泌,而二甲双胍治疗可抑制这种分泌。为了进一步揭示相关机制,我们研究了二甲双胍治疗如何影响 TNF-α 和 IL-17A 刺激激活的 NLRP3 炎性体。我们发现这种治疗下调了 caspase-1 的表达,caspase-1 是 NLRP3 炎症小体的关键介质。此外,AMPK 和 SIRT1 抑制剂消除了二甲双胍治疗诱导的 caspase-1 下调,表明 AMPK 和 SIRT1 对于 NHEK 中 NLRP3 炎性体的抑制作用至关重要。由于 IL-1β 刺激诱导 NHEK 中 IL-36γ、CXCL1、CXCL2、CCL20、S100A7、S100A8 和 S100A9 mRNA 和蛋白水平上调,我们检查了二甲双胍治疗是否影响此类基因表达。二甲双胍治疗抑制 TNF-α 和 IL-17A 刺激诱导的 IL-36γ、CXCL1、CXCL2、CCL20、S100A7、S100A8 和 S100A9 mRNA 和蛋白水平的上调。最后,我们在咪喹莫特诱导的小鼠银屑病模型中检查了二甲双胍给药是否影响银屑病的发展。口服二甲双胍治疗显着降低耳朵厚度、表皮增生和炎症细胞浸润。二甲双胍治疗下表皮细胞因子谱显示,与对照水平相比,IL-1β、Cxcl1、Cxcl2、S100a7、S100a8 和 S100A9 mRNA 水平下调。这些结果表明二甲双胍给药可防止体内银屑病的发展。总的来说,我们的研究结果表明二甲双胍介导的皮肤抗银屑病作用有可能治疗 T2DM 患者的银屑病。











































 京公网安备 11010802027423号
京公网安备 11010802027423号