当前位置:
X-MOL 学术
›
JAMA Pediatr.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Assessment of an Updated Neonatal Research Network Extremely Preterm Birth Outcome Model in the Vermont Oxford Network
JAMA Pediatrics ( IF 24.7 ) Pub Date : 2020-05-04 , DOI: 10.1001/jamapediatrics.2019.6294 Matthew A Rysavy 1 , Jeffrey D Horbar 2, 3 , Edward F Bell 1 , Lei Li 4 , Lucy T Greenberg 2 , Jon E Tyson 5 , Ravi M Patel 6 , Waldemar A Carlo 7 , Noelle E Younge 8 , Charles E Green 5 , Erika M Edwards 2, 9 , Susan R Hintz 10 , Michele C Walsh 11 , Jeffrey S Buzas 9 , Abhik Das 12 , Rosemary D Higgins 13 ,
JAMA Pediatrics ( IF 24.7 ) Pub Date : 2020-05-04 , DOI: 10.1001/jamapediatrics.2019.6294 Matthew A Rysavy 1 , Jeffrey D Horbar 2, 3 , Edward F Bell 1 , Lei Li 4 , Lucy T Greenberg 2 , Jon E Tyson 5 , Ravi M Patel 6 , Waldemar A Carlo 7 , Noelle E Younge 8 , Charles E Green 5 , Erika M Edwards 2, 9 , Susan R Hintz 10 , Michele C Walsh 11 , Jeffrey S Buzas 9 , Abhik Das 12 , Rosemary D Higgins 13 ,
Affiliation
|
Importance
The Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network (NRN) extremely preterm birth outcome model is widely used for prognostication by practitioners caring for families expecting extremely preterm birth. The model provides information on mean outcomes from 1998 to 2003 and does not account for substantial variation in outcomes among US hospitals. Objective
To update and validate the NRN extremely preterm birth outcome model for most extremely preterm infants in the United States. Design, Setting, and Participants
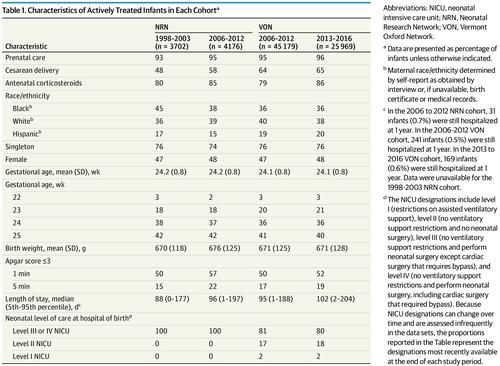
This prognostic study included 3 observational cohorts from January 1, 2006, to December 31, 2016, at 19 US centers in the NRN (derivation cohort) and 637 US centers in Vermont Oxford Network (VON) (validation cohorts). Actively treated infants born at 22 weeks' 0 days' to 25 weeks' 6 days' gestation and weighing 401 to 1000 g, including 4176 in the NRN for 2006 to 2012, 45 179 in VON for 2006 to 2012, and 25 969 in VON for 2013 to 2016, were studied. VON cohorts comprised more than 85% of eligible US births. Data analysis was performed from May 1, 2017, to March 31, 2019. Exposures
Predictive variables used in the original model, including infant sex, birth weight, plurality, gestational age at birth, and exposure to antenatal corticosteroids. Main Outcomes and Measures
The main outcome was death before discharge. Secondary outcomes included neurodevelopmental impairment at 18 to 26 months' corrected age and measures of hospital resource use (days of hospitalization and ventilator use). Results
Among 4176 actively treated infants in the NRN cohort (48% female; mean [SD] gestational age, 24.2 [0.8] weeks), survival was 63% vs 62% among 3702 infants in the era of the original model (47% female; mean [SD] gestational age, 24.2 [0.8] weeks). In the concurrent (2006-2012) VON cohort, survival was 66% among 45 179 actively treated infants (47% female; mean [SD] gestational age, 24.1 [0.8] weeks) and 70% among 25 969 infants from 2013 to 2016 (48% female; mean [SD] gestational age, 24.1 [0.8] weeks). Model C statistics were 0.74 in the 2006-2012 validation cohort and 0.73 in the 2013-2016 validation cohort. With the use of decision curve analysis to compare the model with a gestational age-only approach to prognostication, the updated model showed a predictive advantage. The birth hospital contributed equally as much to prediction of survival as gestational age (20%) but less than the other factors combined (60%). Conclusions and Relevance
An updated model using well-known factors to predict survival for extremely preterm infants performed moderately well when applied to large US cohorts. Because survival rates change over time, the model requires periodic updating. The hospital of birth contributed substantially to outcome prediction.
中文翻译:

佛蒙特州牛津网络中更新的新生儿研究网络极早产结果模型的评估
重要性 Eunice Kennedy Shriver 国家儿童健康与人类发展研究所新生儿研究网络 (NRN) 极早产结果模型广泛用于护理极早产家庭的从业者进行预测。该模型提供了 1998 年至 2003 年平均结果的信息,并未考虑美国医院之间结果的显着差异。目的 更新和验证美国大多数极早产儿的 NRN 极早产结局模型。设计、设置和参与者 这项预后研究包括 2006 年 1 月 1 日至 2016 年 12 月 31 日在 NRN 的 19 个美国中心(推导队列)和佛蒙特州牛津网络 (VON) 的 637 个美国中心(验证队列)的 3 个观察性队列)。积极治疗 22 周出生的婴儿 0 天至 25 周 6 天妊娠,体重 401 至 1000 g,其中 2006 至 2012 年 NRN 4176,2006 至 2012 年 VON 45 179,2016 年 VON 25 969 至 2. VON 队列占符合条件的美国出生人数的 85% 以上。数据分析时间为 2017 年 5 月 1 日至 2019 年 3 月 31 日。 暴露 原始模型中使用的预测变量,包括婴儿性别、出生体重、多胞胎、出生胎龄和产前皮质类固醇暴露。主要结果和措施主要结果是出院前死亡。次要结果包括 18 至 26 个月矫正年龄时的神经发育障碍和医院资源使用量(住院天数和呼吸机使用天数)。结果 在 NRN 队列中 4176 名积极治疗的婴儿中(48% 为女性;平均 [SD] 胎龄,24.2 [0.8] 周),原始模型时代 3702 名婴儿的存活率为 63% 与 62%(47% 为女性;平均 [SD] 胎龄,24.2 [0.8] 周)。在同期(2006-2012 年)VON 队列中,45179 名积极治疗的婴儿(47% 为女性;平均 [SD] 胎龄,24.1 [0.8] 周)的存活率为 66%,2013 年至 2016 年的 25969 名婴儿的存活率为 70% (48% 的女性;平均 [SD] 胎龄,24.1 [0.8] 周)。模型 C 统计数据在 2006-2012 验证队列中为 0.74,在 2013-2016 验证队列中为 0.73。通过使用决策曲线分析将模型与仅孕龄预测方法进行比较,更新后的模型显示出预测优势。分娩医院对生存预测的贡献与胎龄 (20%) 相同,但低于其他因素的总和 (60%)。结论和相关性 使用众所周知的因素来预测极早产儿存活率的更新模型在应用于大型美国队列时表现中等。由于存活率随时间变化,因此模型需要定期更新。出生医院对结果预测做出了重大贡献。
更新日期:2020-05-04
中文翻译:

佛蒙特州牛津网络中更新的新生儿研究网络极早产结果模型的评估
重要性 Eunice Kennedy Shriver 国家儿童健康与人类发展研究所新生儿研究网络 (NRN) 极早产结果模型广泛用于护理极早产家庭的从业者进行预测。该模型提供了 1998 年至 2003 年平均结果的信息,并未考虑美国医院之间结果的显着差异。目的 更新和验证美国大多数极早产儿的 NRN 极早产结局模型。设计、设置和参与者 这项预后研究包括 2006 年 1 月 1 日至 2016 年 12 月 31 日在 NRN 的 19 个美国中心(推导队列)和佛蒙特州牛津网络 (VON) 的 637 个美国中心(验证队列)的 3 个观察性队列)。积极治疗 22 周出生的婴儿 0 天至 25 周 6 天妊娠,体重 401 至 1000 g,其中 2006 至 2012 年 NRN 4176,2006 至 2012 年 VON 45 179,2016 年 VON 25 969 至 2. VON 队列占符合条件的美国出生人数的 85% 以上。数据分析时间为 2017 年 5 月 1 日至 2019 年 3 月 31 日。 暴露 原始模型中使用的预测变量,包括婴儿性别、出生体重、多胞胎、出生胎龄和产前皮质类固醇暴露。主要结果和措施主要结果是出院前死亡。次要结果包括 18 至 26 个月矫正年龄时的神经发育障碍和医院资源使用量(住院天数和呼吸机使用天数)。结果 在 NRN 队列中 4176 名积极治疗的婴儿中(48% 为女性;平均 [SD] 胎龄,24.2 [0.8] 周),原始模型时代 3702 名婴儿的存活率为 63% 与 62%(47% 为女性;平均 [SD] 胎龄,24.2 [0.8] 周)。在同期(2006-2012 年)VON 队列中,45179 名积极治疗的婴儿(47% 为女性;平均 [SD] 胎龄,24.1 [0.8] 周)的存活率为 66%,2013 年至 2016 年的 25969 名婴儿的存活率为 70% (48% 的女性;平均 [SD] 胎龄,24.1 [0.8] 周)。模型 C 统计数据在 2006-2012 验证队列中为 0.74,在 2013-2016 验证队列中为 0.73。通过使用决策曲线分析将模型与仅孕龄预测方法进行比较,更新后的模型显示出预测优势。分娩医院对生存预测的贡献与胎龄 (20%) 相同,但低于其他因素的总和 (60%)。结论和相关性 使用众所周知的因素来预测极早产儿存活率的更新模型在应用于大型美国队列时表现中等。由于存活率随时间变化,因此模型需要定期更新。出生医院对结果预测做出了重大贡献。









































 京公网安备 11010802027423号
京公网安备 11010802027423号