Gastroenterology ( IF 25.7 ) Pub Date : 2020-02-25 , DOI: 10.1053/j.gastro.2020.02.032 Bharati Kochar 1 , Winston Cai 2 , Andrew Cagan 3 , Ashwin N Ananthakrishnan 1
|
Background & Aims
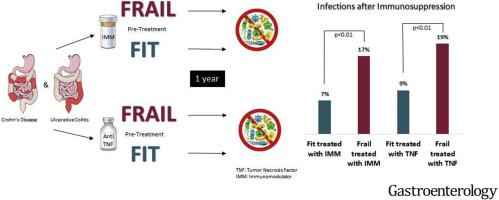
Infections are an important adverse effect of immunosuppression for treatment of inflammatory bowel diseases (IBDs). However, risk of infection cannot be sufficiently determined based on patients’ ages or comorbidities. Frailty has been associated with outcomes of patients with other inflammatory diseases. We aimed to determine the association between frailty and risk of infections after immunosuppression for IBD.
Methods
We performed a cohort study of 11,001 patients with IBD, using a validated frailty definition based on International Classification of Disease codes to identify patients who were frail vs fit in the 2 years before initiation of an anti–tumor necrosis factor (TNF) or immunomodulator therapy, from 1996 through 2010. Our primary outcome was an infection in the first year after treatment. We constructed multivariable logistic regression models, adjusting for clinically pertinent confounders (age, comorbidities, steroid use, and combination therapy) to determine the association between frailty and posttreatment infections.
Results
There were 1299 patients treated with an anti-TNF agent and 2676 patients treated with an immunomodulator. In this cohort, 5% of patients who received anti-TNF therapy and 7% of patients who received an immunomodulator were frail in the 2 years before immunosuppression. Frail patients were older and had more comorbidities. Higher proportions of frail patients developed infections after treatment (19% after TNF and 17% after immunomodulators) compared with fit patients (9% after TNF and 7% after immunomodulators; P < .01 for frail vs fit in both groups). Frail patients had an increased risk of infection after we adjusted for age, comorbidities, and concomitant medications (anti-TNF adjusted odds ratio, 2.05 [95% confidence interval, 1.07–3.93] and immunomodulator adjusted odds ratio, 1.81 [95% confidence interval, 1.22–2.70]).
Conclusions
Frailty was associated with infections after immunosuppression in patients with IBD after we adjust for age and comorbidities. Systematic assessment and strategies to improve frailty might reduce infection risk in patients with IBD.
中文翻译:

炎症性肠病患者的免疫抑制后,治疗前的虚弱与感染风险的增加独立相关。
背景与目标
感染是免疫抑制治疗炎症性肠病(IBD)的重要不利影响。但是,不能根据患者的年龄或合并症充分确定感染的风险。虚弱与其他炎症性疾病患者的预后有关。我们旨在确定免疫抑制IBD后虚弱与感染风险之间的关联。
方法
我们对11,001名IBD患者进行了一项队列研究,使用了基于国际疾病分类代码的经过验证的脆弱定义,以确定在开始抗肿瘤坏死因子(TNF)或免疫调节剂治疗之前的2年中,脆弱与健康的患者,从1996年到2010年。我们的主要结局是治疗后第一年出现感染。我们构建了多变量logistic回归模型,并针对临床相关的混杂因素(年龄,合并症,类固醇使用和联合治疗)进行了调整,以确定脆弱与治疗后感染之间的关联。
结果
有1299例接受抗TNF药物治疗的患者和2676例接受了免疫调节剂的患者。在该队列中,免疫抑制前2年中接受抗TNF治疗的患者有5%,接受免疫调节剂的患者有7%。体弱的患者年龄较大,合并症更多。体弱患者的更高比例配合与患者(TNF后9%和免疫后7%比较处理(TNF后19%和免疫后17%)之后开发的感染; P 两组的体弱vs. <0.01。调整年龄,合并症和并用药物后,体弱患者的感染风险增加(抗TNF调整比值比2.05 [95%置信区间1.07-3.93]和免疫调节剂调整比值比1.81 [95%置信区间] ,1.22–2.70])。
结论
调整年龄和合并症后,IBD患者免疫抑制后虚弱与感染相关。系统性评估和改善脆弱性的策略可能会降低IBD患者的感染风险。









































 京公网安备 11010802027423号
京公网安备 11010802027423号