The Lancet HIV ( IF 12.8 ) Pub Date : 2020-02-24 , DOI: 10.1016/s2352-3018(19)30402-3 Paul K Drain 1 , Jienchi Dorward 2 , Lauren R Violette 3 , Justice Quame-Amaglo 4 , Katherine K Thomas 4 , Natasha Samsunder 5 , Hope Ngobese 6 , Koleka Mlisana 7 , Pravikrishnen Moodley 8 , Deborah Donnell 4 , Ruanne V Barnabas 9 , Kogieleum Naidoo 10 , Salim S Abdool Karim 11 , Connie Celum 9 , Nigel Garrett 12
|
Background
Monitoring HIV treatment with laboratory testing introduces delays for providing appropriate care in resource-limited settings. The aim of our study was to determine whether point-of-care HIV viral load testing with task shifting changed treatment and care outcomes for adults on antiretroviral therapy (ART) when compared with standard laboratory viral load testing.
Methods
We did an open-label, non-inferiority, randomised controlled trial in a public clinic in Durban, South Africa. We enrolled HIV-positive adults (aged ≥18 years) who presented for their first routine HIV viral load test 6 months after ART initiation. Individuals were randomly assigned by a random number allocation sequence to receive either point-of-care viral load testing at enrolment and after 6 months with task shifting to enrolled nurses (intervention group), or laboratory viral load testing (standard-of-care group). The primary outcome was combined viral suppression (<200 copies per mL) and retention at 12 months after enrolment. A non-inferiority margin of 10% was used. Analysis was done by intention to treat. This study was registered with ClinicalTrials.gov, NCT03066128.
Findings
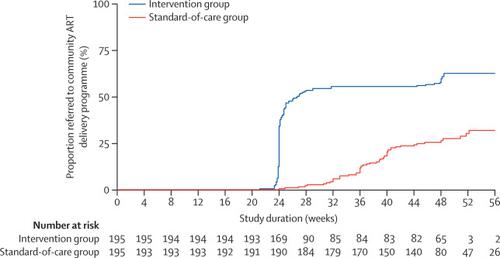
Between Feb 24, 2017, and Aug 23, 2017, we screened 657 participants, and 390 were enrolled and randomly assigned to either the intervention group (n=195) or standard-of-care group (n=195). 175 (90%) individuals in the intervention group and 148 (76%) individuals in the standard-of-care group had the primary outcome of retention with viral suppression, a difference of 13·9% (95% CI 6·4–21·2; p<0·00040). 182 participants (93%) in the intervention group had viral suppression compared with 162 (83%) in the standard-of-care group (difference 10·3%, 3·9–16·8; p=0·0025); 180 (92%) and 162 (85%) were retained in care (7·7%, 1·3–14·2; p=0·026). There were no adverse events related to point-of-care HIV viral load testing or task shifting.
Interpretation
Point-of-care viral load testing combined with task shifting significantly improved viral suppression and retention in HIV care. Point-of-care testing can simplify treatment and improve outcomes for HIV-positive adults receiving ART in resource-limited settings.
Funding
National Institute of Allergy and Infectious Diseases.
中文翻译:

护理点HIV病毒载量测试与任务转移相结合以改善治疗效果(STREAM):一项开放性,非劣效性,随机对照试验的发现。
背景
用实验室测试监测HIV治疗会延误在资源有限的环境中提供适当护理的时间。我们研究的目的是确定与标准实验室病毒载量测试相比,通过任务转移进行的护理点HIV病毒载量测试是否改变了接受抗逆转录病毒疗法(ART)的成年人的治疗和护理效果。
方法
我们在南非德班的一家公共诊所进行了一项开放性,非自卑性,随机对照试验。我们招募了HIV阳性成人(≥18岁),他们在接受抗逆转录病毒治疗6个月后首次进行了常规HIV病毒载量测试。按照随机数字分配顺序对个体进行随机分配,以在入组时以及在任务转移至入组护士的情况下进行6个月后即刻进行护理点病毒载量测试(干预组),或在实验室进行病毒载量测试(照护标准组) )。主要结局是合并病毒抑制(每毫升<200拷贝)和入选后12个月保留。使用非劣质性余量为10%。分析是按意向进行的。该研究已在ClinicalTrials.gov注册,NCT03066128。
发现
在2017年2月24日至2017年8月23日之间,我们筛选了657名参与者,并招募了390名参与者,并将其随机分配至干预组(n = 195)或护理标准组(n = 195)。干预组中有175(90%)个人和标准护理组中有148(76%)个人具有病毒抑制的主要保留结果,相差13·9%(95%CI 6·4– 21·2; p <0·00040)。干预组有182名参与者(93%)受到病毒抑制,而标准护理组有162名参与者(83%)(差异10·3%,3·9–16·8; p = 0·0025); 分别有180名(92%)和162名(85%)接受了护理(7·7%,1·3-14·2; p = 0·026)。没有与护理点HIV病毒载量测试或任务转移相关的不良事件。
解释
即时护理病毒载量测试与任务转移相结合,可以显着改善病毒抑制和在HIV护理中的保留率。对于在资源有限的环境中接受抗逆转录病毒治疗的艾滋病毒呈阳性的成年人,现场护理测试可以简化治疗并改善结果。
资金
美国国家过敏和传染病研究所。











































 京公网安备 11010802027423号
京公网安备 11010802027423号