当前位置:
X-MOL 学术
›
JAMA Pediatr.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Neonatal Mortality After Interhospital Transfer of Pregnant Women for Imminent Very Preterm Birth in Illinois
JAMA Pediatrics ( IF 24.7 ) Pub Date : 2020-04-01 , DOI: 10.1001/jamapediatrics.2019.6055 Kshama P Shah 1 , Raye-Ann O deRegnier 1 , William A Grobman 2 , Amanda C Bennett 3
JAMA Pediatrics ( IF 24.7 ) Pub Date : 2020-04-01 , DOI: 10.1001/jamapediatrics.2019.6055 Kshama P Shah 1 , Raye-Ann O deRegnier 1 , William A Grobman 2 , Amanda C Bennett 3
Affiliation
|
Importance
Reducing neonatal mortality is a national health care priority. Understanding the association between neonatal mortality and antenatal transfer of pregnant women to a level III perinatal hospital for delivery of infants who are very preterm (VPT) may help identify opportunities for improvement. Objective
To assess whether antenatal transfer to a level III hospital is associated with neonatal mortality in infants who are VPT. Design, Setting, and Participants
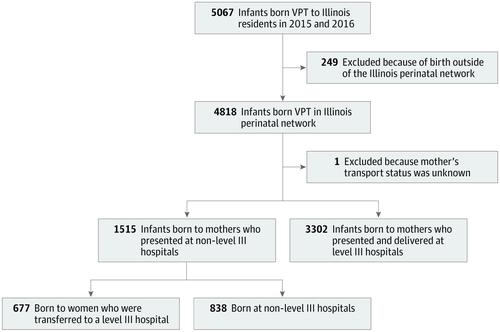
This population-based cross-sectional study included infants who were born VPT to Illinois residents in Illinois perinatal-network hospitals between January 1, 2015, and December 31, 2016, and followed up for 28 days after birth. Data analysis was conducted from June 2017 to September 2018. Exposures
Delivery of an infant who was VPT at a (1) level III hospital after maternal presentation at that hospital (reference group), (2) a level III hospital after antenatal (in utero) transfer from another hospital, or (3) a non-level III hospital. Main Outcomes and Measures
Neonatal mortality. Results
The study included 4817 infants who were VPT (gestational age, 22-31 completed weeks) and were born to Illinois residents in 2015 and 2016. Of those, 3302 infants (68.5%) were born at a level III hospital after maternal presentation at that hospital, 677 (14.1%) were born at a level III hospital after antenatal transfer, and 838 (17.4%) were born at a non-level III hospital. Neonatal mortality for all infants who were VPT included in this study was 573 of 4817 infants (11.9%). The neonatal mortality was 10.7% for the reference group (362 of 3302 infants), 9.8% for the antenatal transfer group (66 of 677 infants), and 17.3% for the non-level III birth group (145 of 838 infants). When adjusted for significant social and medical characteristics, infants born VPT at a level III hospital after antenatal transfer from another facility had a similar risk of neonatal mortality as infants born at a level III hospital (odds ratio, 0.79 [95% CI, 0.56-1.13]) after maternal presentation at the same hospital. Infants born at a non-level III hospital had an increased risk of neonatal mortality compared with infants born at a level III hospital after maternal presentation to the same hospital (odds ratio, 1.52 [95% CI, 1.14-2.02]). Conclusions and Relevance
The risk of neonatal mortality was similar for infants who were VPT, whether women initially presented at a level III hospital or were transferred to a level III hospital before delivery. This suggests that the increased risk of mortality associated with delivery at a non-level III hospital may be mitigated by optimizing opportunities for early maternal transfer to a level III hospital.
中文翻译:

伊利诺伊州即将出生的极早产孕妇院内转运后的新生儿死亡率
重要性 降低新生儿死亡率是国家卫生保健的优先事项。了解新生儿死亡率与孕妇产前转移至三级围产期医院以接生极早产儿 (VPT) 之间的关联可能有助于确定改进机会。目的 评估产前转至三级医院是否与 VPT 婴儿的新生儿死亡率相关。设计、设置和参与者 这项基于人群的横断面研究包括在 2015 年 1 月 1 日至 2016 年 12 月 31 日期间在伊利诺伊州围产期网络医院出生的伊利诺伊州居民 VPT,并在出生后随访 28 天。数据分析于2017年6月至2018年9月进行。暴露 在 (1) 三级医院(参考组)产妇就诊后在三级医院分娩的 VPT 婴儿,(2)从另一家医院进行产前(子宫内)转移后在三级医院分娩,或 (3)非三级医院。主要结果和措施 新生儿死亡率。结果 该研究包括 4817 名 VPT(胎龄,22-31 周)婴儿,他们在 2015 年和 2016 年出生于伊利诺伊州居民。其中 3302 名婴儿(68.5%)在那家医院,677人(14.1%)产前转后出生在三级医院,838人(17.4%)出生在非三级医院。本研究中包括的所有 VPT 婴儿的新生儿死亡率为 4817 名婴儿中的 573 名 (11.9%)。新生儿死亡率为10。参考组(3302 名婴儿中的 362 名)为 7%,产前转移组(677 名婴儿中的 66 名)为 9.8%,非 III 级出生组(838 名婴儿中的 145 名)为 17.3%。当针对显着的社会和医学特征进行调整后,从另一家医院进行产前转移后在三级医院出生的 VPT 婴儿与在三级医院出生的婴儿具有相似的新生儿死亡风险(优势比,0.79 [95% CI,0.56- 1.13])在同一家医院的产妇就诊后。与产妇到同一家医院就诊后在三级医院出生的婴儿相比,在非三级医院出生的婴儿新生儿死亡风险增加(优势比,1.52 [95% CI,1.14-2.02])。结论和相关性 VPT 婴儿的新生儿死亡风险相似,妇女最初是在三级医院就诊还是在分娩前被转移到三级医院。这表明,在非三级医院分娩相关的死亡风险增加可以通过优化将产妇早期转移到三级医院的机会来降低。
更新日期:2020-04-01
中文翻译:

伊利诺伊州即将出生的极早产孕妇院内转运后的新生儿死亡率
重要性 降低新生儿死亡率是国家卫生保健的优先事项。了解新生儿死亡率与孕妇产前转移至三级围产期医院以接生极早产儿 (VPT) 之间的关联可能有助于确定改进机会。目的 评估产前转至三级医院是否与 VPT 婴儿的新生儿死亡率相关。设计、设置和参与者 这项基于人群的横断面研究包括在 2015 年 1 月 1 日至 2016 年 12 月 31 日期间在伊利诺伊州围产期网络医院出生的伊利诺伊州居民 VPT,并在出生后随访 28 天。数据分析于2017年6月至2018年9月进行。暴露 在 (1) 三级医院(参考组)产妇就诊后在三级医院分娩的 VPT 婴儿,(2)从另一家医院进行产前(子宫内)转移后在三级医院分娩,或 (3)非三级医院。主要结果和措施 新生儿死亡率。结果 该研究包括 4817 名 VPT(胎龄,22-31 周)婴儿,他们在 2015 年和 2016 年出生于伊利诺伊州居民。其中 3302 名婴儿(68.5%)在那家医院,677人(14.1%)产前转后出生在三级医院,838人(17.4%)出生在非三级医院。本研究中包括的所有 VPT 婴儿的新生儿死亡率为 4817 名婴儿中的 573 名 (11.9%)。新生儿死亡率为10。参考组(3302 名婴儿中的 362 名)为 7%,产前转移组(677 名婴儿中的 66 名)为 9.8%,非 III 级出生组(838 名婴儿中的 145 名)为 17.3%。当针对显着的社会和医学特征进行调整后,从另一家医院进行产前转移后在三级医院出生的 VPT 婴儿与在三级医院出生的婴儿具有相似的新生儿死亡风险(优势比,0.79 [95% CI,0.56- 1.13])在同一家医院的产妇就诊后。与产妇到同一家医院就诊后在三级医院出生的婴儿相比,在非三级医院出生的婴儿新生儿死亡风险增加(优势比,1.52 [95% CI,1.14-2.02])。结论和相关性 VPT 婴儿的新生儿死亡风险相似,妇女最初是在三级医院就诊还是在分娩前被转移到三级医院。这表明,在非三级医院分娩相关的死亡风险增加可以通过优化将产妇早期转移到三级医院的机会来降低。











































 京公网安备 11010802027423号
京公网安备 11010802027423号