当前位置:
X-MOL 学术
›
JAMA Intern. Med.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Empirical Anti-MRSA vs Standard Antibiotic Therapy and Risk of 30-Day Mortality in Patients Hospitalized for Pneumonia
JAMA Internal Medicine ( IF 22.5 ) Pub Date : 2020-04-01 , DOI: 10.1001/jamainternmed.2019.7495 Barbara Ellen Jones 1, 2 , Jian Ying 3 , Vanessa Stevens 2, 4 , Candace Haroldsen 3 , Tao He 3 , McKenna Nevers 3 , Matthew A Christensen 5 , Richard E Nelson 2, 6 , Gregory J Stoddard 3 , Brian C Sauer 2, 4 , Peter M Yarbrough 2, 7 , Makoto M Jones 2, 4 , Matthew Bidwell Goetz 8 , Tom Greene 3 , Matthew H Samore 2, 4
JAMA Internal Medicine ( IF 22.5 ) Pub Date : 2020-04-01 , DOI: 10.1001/jamainternmed.2019.7495 Barbara Ellen Jones 1, 2 , Jian Ying 3 , Vanessa Stevens 2, 4 , Candace Haroldsen 3 , Tao He 3 , McKenna Nevers 3 , Matthew A Christensen 5 , Richard E Nelson 2, 6 , Gregory J Stoddard 3 , Brian C Sauer 2, 4 , Peter M Yarbrough 2, 7 , Makoto M Jones 2, 4 , Matthew Bidwell Goetz 8 , Tom Greene 3 , Matthew H Samore 2, 4
Affiliation
|
Importance
Use of empirical broad-spectrum antibiotics for pneumonia has increased owing to concern for resistant organisms, including methicillin-resistant Staphylococcus aureus (MRSA). The association of empirical anti-MRSA therapy with outcomes among patients with pneumonia is unknown, even for high-risk patients. Objective
To compare 30-day mortality among patients hospitalized for pneumonia receiving empirical anti-MRSA therapy vs standard empirical antibiotic regimens. Design, Setting, and Participants
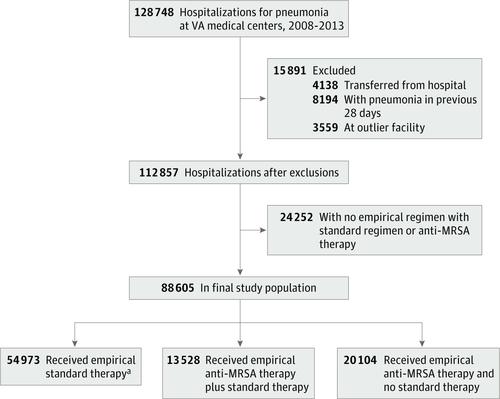
Retrospective multicenter cohort study was conducted of all hospitalizations in which patients received either anti-MRSA or standard therapy for community-onset pneumonia in the Veterans Health Administration health care system from January 1, 2008, to December 31, 2013. Subgroups of patients analyzed were those with initial intensive care unit admission, MRSA risk factors, positive results of a MRSA surveillance test, and positive results of a MRSA admission culture. Primary analysis was an inverse probability of treatment-weighted propensity score analysis using generalized estimating equation regression; secondary analyses included an instrumental variable analysis. Statistical analysis was conducted from June 14 to November 20, 2019. Exposures
Empirical anti-MRSA therapy plus standard pneumonia therapy vs standard therapy alone within the first day of hospitalization. Main Outcomes and Measures
Risk of 30-day all-cause mortality after adjustment for patient comorbidities, vital signs, and laboratory results. Secondary outcomes included the development of kidney injury and secondary infections with Clostridioides difficile, vancomycin-resistant Enterococcus species, or gram-negative bacilli. Results
Among 88 605 hospitalized patients (86 851 men; median age, 70 years [interquartile range, 62-81 years]), empirical anti-MRSA therapy was administered to 33 632 (38%); 8929 patients (10%) died within 30 days. Compared with standard therapy alone, in weighted propensity score analysis, empirical anti-MRSA therapy plus standard therapy was significantly associated with an increased adjusted risk of death (adjusted risk ratio [aRR], 1.4 [95% CI, 1.3-1.5]), kidney injury (aRR, 1.4 [95% CI, 1.3-1.5]), and secondary C difficile infections (aRR, 1.6 [95% CI, 1.3-1.9]), vancomycin-resistant Enterococcus spp infections (aRR, 1.6 [95% CI, 1.0-2.3]), and secondary gram-negative rod infections (aRR, 1.5 [95% CI, 1.2-1.8]). Similar associations between anti-MRSA therapy use and 30-day mortality were found by instrumental variable analysis (aRR, 1.6 [95% CI, 1.4-1.9]) and among patients admitted to the intensive care unit (aRR, 1.3 [95% CI, 1.2-1.5]), those with a high risk for MRSA (aRR, 1.2 [95% CI, 1.1-1.4]), and those with MRSA detected on surveillance testing (aRR, 1.6 [95% CI, 1.3-1.9]). No significant favorable association was found between empirical anti-MRSA therapy and death among patients with MRSA detected on culture (aRR, 1.1 [95% CI, 0.8-1.4]). Conclusions and Relevance
This study suggests that empirical anti-MRSA therapy was not associated with reduced mortality for any group of patients hospitalized for pneumonia. These results contribute to a growing body of evidence that questions the value of empirical use of anti-MRSA therapy using existing risk approaches.
中文翻译:

肺炎住院患者的经验性抗 MRSA 与标准抗生素治疗和 30 天死亡率风险
重要性 由于对耐药微生物的担忧,包括耐甲氧西林金黄色葡萄球菌 (MRSA),经验性广谱抗生素在肺炎中的使用有所增加。经验性抗 MRSA 治疗与肺炎患者预后的关联尚不清楚,即使对于高危患者也是如此。目的 比较接受经验性抗 MRSA 治疗与标准经验性抗生素治疗的肺炎住院患者的 30 天死亡率。设计、设置和参与者 对 2008 年 1 月 1 日至 2013 年 12 月 31 日在退伍军人健康管理局医疗保健系统中接受抗 MRSA 或社区发病肺炎标准治疗的所有住院患者进行了回顾性多中心队列研究. 所分析的患者亚组包括最初入住重症监护病房、MRSA 危险因素、MRSA 监测检测阳性结果和 MRSA 入院培养阳性结果的患者。主要分析是使用广义估计方程回归的治疗加权倾向评分分析的逆概率;二次分析包括工具变量分析。统计分析于 2019 年 6 月 14 日至 11 月 20 日进行。 暴露 住院第一天内经验性抗 MRSA 治疗加标准肺炎治疗 vs 单独标准治疗。主要结果和措施 调整患者合并症、生命体征和实验室结果后 30 天全因死亡率的风险。次要结局包括肾损伤的发展和艰难梭菌、耐万古霉素肠球菌或革兰氏阴性杆菌的继发感染。结果 在 88 605 名住院患者(86 851 名男性;中位年龄 70 岁 [四分位距,62-81 岁])中,33 632 名(38%)接受了经验性抗 MRSA 治疗;8929 名患者(10%)在 30 天内死亡。与单独标准治疗相比,在加权倾向评分分析中,经验性抗 MRSA 治疗加标准治疗与调整后死亡风险增加显着相关(调整后风险比 [aRR],1.4 [95% CI,1.3-1.5]),肾损伤(aRR,1.4 [95% CI,1.3-1.5])和继发性艰难梭菌感染(aRR,1.6 [95% CI,1.3-1.9]),耐万古霉素肠球菌属感染(aRR,1.6 [95%] CI, 1.0-2.3]), 和继发性革兰氏阴性杆菌感染(aRR,1.5 [95% CI,1.2-1.8])。通过工具变量分析(aRR,1.6 [95% CI,1.4-1.9])和入住重症监护病房的患者(aRR,1.3 [95% CI])发现抗 MRSA 治疗使用与 30 天死亡率之间存在类似关联, 1.2-1.5])、MRSA 高风险者 (aRR, 1.2 [95% CI, 1.1-1.4]),以及监测检测发现 MRSA 者 (aRR, 1.6 [95% CI, 1.3-1.9] )。在培养检测到 MRSA 的患者中,经验性抗 MRSA 治疗与死亡之间没有发现显着的有利关联(aRR,1.1 [95% CI,0.8-1.4])。结论和相关性 该研究表明,对于任何因肺炎住院的患者,经验性抗 MRSA 治疗与降低死亡率无关。
更新日期:2020-04-01
中文翻译:

肺炎住院患者的经验性抗 MRSA 与标准抗生素治疗和 30 天死亡率风险
重要性 由于对耐药微生物的担忧,包括耐甲氧西林金黄色葡萄球菌 (MRSA),经验性广谱抗生素在肺炎中的使用有所增加。经验性抗 MRSA 治疗与肺炎患者预后的关联尚不清楚,即使对于高危患者也是如此。目的 比较接受经验性抗 MRSA 治疗与标准经验性抗生素治疗的肺炎住院患者的 30 天死亡率。设计、设置和参与者 对 2008 年 1 月 1 日至 2013 年 12 月 31 日在退伍军人健康管理局医疗保健系统中接受抗 MRSA 或社区发病肺炎标准治疗的所有住院患者进行了回顾性多中心队列研究. 所分析的患者亚组包括最初入住重症监护病房、MRSA 危险因素、MRSA 监测检测阳性结果和 MRSA 入院培养阳性结果的患者。主要分析是使用广义估计方程回归的治疗加权倾向评分分析的逆概率;二次分析包括工具变量分析。统计分析于 2019 年 6 月 14 日至 11 月 20 日进行。 暴露 住院第一天内经验性抗 MRSA 治疗加标准肺炎治疗 vs 单独标准治疗。主要结果和措施 调整患者合并症、生命体征和实验室结果后 30 天全因死亡率的风险。次要结局包括肾损伤的发展和艰难梭菌、耐万古霉素肠球菌或革兰氏阴性杆菌的继发感染。结果 在 88 605 名住院患者(86 851 名男性;中位年龄 70 岁 [四分位距,62-81 岁])中,33 632 名(38%)接受了经验性抗 MRSA 治疗;8929 名患者(10%)在 30 天内死亡。与单独标准治疗相比,在加权倾向评分分析中,经验性抗 MRSA 治疗加标准治疗与调整后死亡风险增加显着相关(调整后风险比 [aRR],1.4 [95% CI,1.3-1.5]),肾损伤(aRR,1.4 [95% CI,1.3-1.5])和继发性艰难梭菌感染(aRR,1.6 [95% CI,1.3-1.9]),耐万古霉素肠球菌属感染(aRR,1.6 [95%] CI, 1.0-2.3]), 和继发性革兰氏阴性杆菌感染(aRR,1.5 [95% CI,1.2-1.8])。通过工具变量分析(aRR,1.6 [95% CI,1.4-1.9])和入住重症监护病房的患者(aRR,1.3 [95% CI])发现抗 MRSA 治疗使用与 30 天死亡率之间存在类似关联, 1.2-1.5])、MRSA 高风险者 (aRR, 1.2 [95% CI, 1.1-1.4]),以及监测检测发现 MRSA 者 (aRR, 1.6 [95% CI, 1.3-1.9] )。在培养检测到 MRSA 的患者中,经验性抗 MRSA 治疗与死亡之间没有发现显着的有利关联(aRR,1.1 [95% CI,0.8-1.4])。结论和相关性 该研究表明,对于任何因肺炎住院的患者,经验性抗 MRSA 治疗与降低死亡率无关。









































 京公网安备 11010802027423号
京公网安备 11010802027423号