Our official English website, www.x-mol.net, welcomes your feedback! (Note: you will need to create a separate account there.)
Association of Physician Orders for Life-Sustaining Treatment With ICU Admission Among Patients Hospitalized Near the End of Life
JAMA ( IF 120.7 ) Pub Date : 2020-03-10 , DOI: 10.1001/jama.2019.22523 Robert Y Lee 1, 2 , Lyndia C Brumback 1, 3 , Seelwan Sathitratanacheewin 1, 4 , William B Lober 1, 5, 6 , Matthew E Modes 1, 2 , Ylinne T Lynch 2 , Corey I Ambrose 7 , James Sibley 1, 5, 6 , Kelly C Vranas 8, 9 , Donald R Sullivan 8, 9 , Ruth A Engelberg 1, 2 , J Randall Curtis 1, 2, 5, 10 , Erin K Kross 1, 2
JAMA ( IF 120.7 ) Pub Date : 2020-03-10 , DOI: 10.1001/jama.2019.22523 Robert Y Lee 1, 2 , Lyndia C Brumback 1, 3 , Seelwan Sathitratanacheewin 1, 4 , William B Lober 1, 5, 6 , Matthew E Modes 1, 2 , Ylinne T Lynch 2 , Corey I Ambrose 7 , James Sibley 1, 5, 6 , Kelly C Vranas 8, 9 , Donald R Sullivan 8, 9 , Ruth A Engelberg 1, 2 , J Randall Curtis 1, 2, 5, 10 , Erin K Kross 1, 2
Affiliation
|
Importance
Patients with chronic illness frequently use Physician Orders for Life-Sustaining Treatment (POLST) to document treatment limitations. Objectives
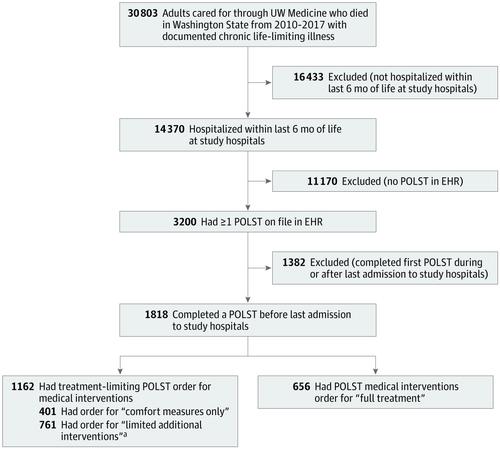
To evaluate the association between POLST order for medical interventions and intensive care unit (ICU) admission for patients hospitalized near the end of life. Design, Setting, and Participants
Retrospective cohort study of patients with POLSTs and with chronic illness who died between January 1, 2010, and December 31, 2017, and were hospitalized 6 months or less before death in a 2-hospital academic health care system. Exposures
POLST order for medical interventions ("comfort measures only" vs "limited additional interventions" vs "full treatment"), age, race/ethnicity, education, days from POLST completion to admission, histories of cancer or dementia, and admission for traumatic injury. Main Outcomes and Measures
The primary outcome was the association between POLST order and ICU admission during the last hospitalization of life; the secondary outcome was receipt of a composite of 4 life-sustaining treatments: mechanical ventilation, vasopressors, dialysis, and cardiopulmonary resuscitation. For evaluating factors associated with POLST-discordant care, the outcome was ICU admission contrary to POLST order for medical interventions during the last hospitalization of life. Results
Among 1818 decedents (mean age, 70.8 [SD, 14.7] years; 41% women), 401 (22%) had POLST orders for comfort measures only, 761 (42%) had orders for limited additional interventions, and 656 (36%) had orders for full treatment. ICU admissions occurred in 31% (95% CI, 26%-35%) of patients with comfort-only orders, 46% (95% CI, 42%-49%) with limited-interventions orders, and 62% (95% CI, 58%-66%) with full-treatment orders. One or more life-sustaining treatments were delivered to 14% (95% CI, 11%-17%) of patients with comfort-only orders and to 20% (95% CI, 17%-23%) of patients with limited-interventions orders. Compared with patients with full-treatment POLSTs, those with comfort-only and limited-interventions orders were significantly less likely to receive ICU admission (comfort only: 123/401 [31%] vs 406/656 [62%], aRR, 0.53 [95% CI, 0.45-0.62]; limited interventions: 349/761 [46%] vs 406/656 [62%], aRR, 0.79 [95% CI, 0.71-0.87]). Across patients with comfort-only and limited-interventions POLSTs, 38% (95% CI, 35%-40%) received POLST-discordant care. Patients with cancer were significantly less likely to receive POLST-discordant care than those without cancer (comfort only: 41/181 [23%] vs 80/220 [36%], aRR, 0.60 [95% CI, 0.43-0.85]; limited interventions: 100/321 [31%] vs 215/440 [49%], aRR, 0.63 [95% CI, 0.51-0.78]). Patients with dementia and comfort-only orders were significantly less likely to receive POLST-discordant care than those without dementia (23/111 [21%] vs 98/290 [34%], aRR, 0.44 [95% CI, 0.29-0.67]). Patients admitted for traumatic injury were significantly more likely to receive POLST-discordant care (comfort only: 29/64 [45%] vs 92/337 [27%], aRR, 1.52 [95% CI, 1.08-2.14]; limited interventions: 51/91 [56%] vs 264/670 [39%], aRR, 1.36 [95% CI, 1.09-1.68]). In patients with limited-interventions orders, older age was significantly associated with less POLST-discordant care (aRR, 0.93 per 10 years [95% CI, 0.88-1.00]). Conclusions and Relevance
Among patients with POLSTs and with chronic life-limiting illness who were hospitalized within 6 months of death, treatment-limiting POLSTs were significantly associated with lower rates of ICU admission compared with full-treatment POLSTs. However, 38% of patients with treatment-limiting POLSTs received intensive care that was potentially discordant with their POLST.
中文翻译:

生命末期住院患者的维持生命治疗医师医嘱与入住 ICU 的关联
重要性 慢性病患者经常使用生命维持治疗医嘱 (POLST) 来记录治疗限制。目的 评估医疗干预的 POLST 命令与临近生命终点住院的患者入住重症监护室 (ICU) 之间的关联。设计、设置和参与者 2010 年 1 月 1 日至 2017 年 12 月 31 日期间死亡的 POLST 和慢性病患者的回顾性队列研究,并在 2 家医院学术医疗保健系统中住院 6 个月或更短时间。医疗干预的暴露 POLST 命令(“仅舒适措施”vs“有限的额外干预”vs“全面治疗”)、年龄、种族/民族、教育、从 POLST 完成到入院的天数、癌症或痴呆病史,并因外伤入院。主要结果和措施 主要结果是 POLST 命令与生命最后一次住院期间入住 ICU 之间的关联;次要结果是接受了 4 种维持生命治疗的复合治疗:机械通气、血管加压药、透析和心肺复苏。为了评估与 POLST 不一致护理相关的因素,结果是在生命最后一次住院期间入住 ICU 与 POLST 医疗干预命令相反。结%) 有全面治疗的订单。31% (95% CI, 26%-35%) 的仅接受舒适指令的患者入住 ICU,46% (95% CI, 42%-49%) 有有限干预令,62% (95% CI, 58%-66%) 有全面治疗令。14% (95% CI, 11%-17%) 的患者接受了一种或多种维持生命的治疗,20% (95% CI, 17%-23%)干预令。与接受全面治疗 POLST 的患者相比,接受仅舒适和有限干预命令的患者入住 ICU 的可能性显着降低(仅舒适:123/401 [31%] vs 406/656 [62%],aRR,0.53 [95% CI,0.45-0.62];有限的干预:349/761 [46%] 与 406/656 [62%],aRR,0.79 [95% CI,0.71-0.87])。在仅接受舒适性和有限干预 POLST 的患者中,38%(95% CI,35%-40%)接受了 POLST 不一致的护理。与非癌症患者相比,癌症患者接受 POLST 不一致护理的可能性显着降低(仅舒适度:41/181 [23%] 与 80/220 [36%],aRR,0.60 [95% CI,0.43-0.85];有限干预:100/321 [31%] 与 215/440 [49%],aRR,0.63 [95% CI,0.51-0.78])。与没有痴呆症的患者相比,患有痴呆症和仅接受舒适性命令的患者接受 POLST 不一致护理的可能性显着降低(23/111 [21%] vs 98/290 [34%],aRR,0.44 [95% CI,0.29-0.67] ])。因外伤入院的患者明显更有可能接受 POLST 不一致的护理(仅舒适度:29/64 [45%] vs 92/337 [27%],aRR,1.52 [95% CI,1.08-2.14];干预有限) :51/91 [56%] 与 264/670 [39%],aRR,1.36 [95% CI,1.09-1.68])。在有有限干预令的患者中,年龄较大与较少的 POLST 不一致护理显着相关(aRR,每 10 年为 0.93 [95% CI,0.88-1.00])。结论和相关性 在死亡 6 个月内住院的 POLST 和慢性限制生命疾病的患者中,与全面治疗 POLST 相比,限制治疗的 POLST 与较低的 ICU 入住率显着相关。然而,38% 的治疗限制性 POLST 患者接受了可能与其 POLST 不一致的重症监护。
更新日期:2020-03-10
中文翻译:

生命末期住院患者的维持生命治疗医师医嘱与入住 ICU 的关联
重要性 慢性病患者经常使用生命维持治疗医嘱 (POLST) 来记录治疗限制。目的 评估医疗干预的 POLST 命令与临近生命终点住院的患者入住重症监护室 (ICU) 之间的关联。设计、设置和参与者 2010 年 1 月 1 日至 2017 年 12 月 31 日期间死亡的 POLST 和慢性病患者的回顾性队列研究,并在 2 家医院学术医疗保健系统中住院 6 个月或更短时间。医疗干预的暴露 POLST 命令(“仅舒适措施”vs“有限的额外干预”vs“全面治疗”)、年龄、种族/民族、教育、从 POLST 完成到入院的天数、癌症或痴呆病史,并因外伤入院。主要结果和措施 主要结果是 POLST 命令与生命最后一次住院期间入住 ICU 之间的关联;次要结果是接受了 4 种维持生命治疗的复合治疗:机械通气、血管加压药、透析和心肺复苏。为了评估与 POLST 不一致护理相关的因素,结果是在生命最后一次住院期间入住 ICU 与 POLST 医疗干预命令相反。结%) 有全面治疗的订单。31% (95% CI, 26%-35%) 的仅接受舒适指令的患者入住 ICU,46% (95% CI, 42%-49%) 有有限干预令,62% (95% CI, 58%-66%) 有全面治疗令。14% (95% CI, 11%-17%) 的患者接受了一种或多种维持生命的治疗,20% (95% CI, 17%-23%)干预令。与接受全面治疗 POLST 的患者相比,接受仅舒适和有限干预命令的患者入住 ICU 的可能性显着降低(仅舒适:123/401 [31%] vs 406/656 [62%],aRR,0.53 [95% CI,0.45-0.62];有限的干预:349/761 [46%] 与 406/656 [62%],aRR,0.79 [95% CI,0.71-0.87])。在仅接受舒适性和有限干预 POLST 的患者中,38%(95% CI,35%-40%)接受了 POLST 不一致的护理。与非癌症患者相比,癌症患者接受 POLST 不一致护理的可能性显着降低(仅舒适度:41/181 [23%] 与 80/220 [36%],aRR,0.60 [95% CI,0.43-0.85];有限干预:100/321 [31%] 与 215/440 [49%],aRR,0.63 [95% CI,0.51-0.78])。与没有痴呆症的患者相比,患有痴呆症和仅接受舒适性命令的患者接受 POLST 不一致护理的可能性显着降低(23/111 [21%] vs 98/290 [34%],aRR,0.44 [95% CI,0.29-0.67] ])。因外伤入院的患者明显更有可能接受 POLST 不一致的护理(仅舒适度:29/64 [45%] vs 92/337 [27%],aRR,1.52 [95% CI,1.08-2.14];干预有限) :51/91 [56%] 与 264/670 [39%],aRR,1.36 [95% CI,1.09-1.68])。在有有限干预令的患者中,年龄较大与较少的 POLST 不一致护理显着相关(aRR,每 10 年为 0.93 [95% CI,0.88-1.00])。结论和相关性 在死亡 6 个月内住院的 POLST 和慢性限制生命疾病的患者中,与全面治疗 POLST 相比,限制治疗的 POLST 与较低的 ICU 入住率显着相关。然而,38% 的治疗限制性 POLST 患者接受了可能与其 POLST 不一致的重症监护。



























 京公网安备 11010802027423号
京公网安备 11010802027423号