当前位置:
X-MOL 学术
›
Modern Pathol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Multiparametric in situ imaging of NPM1-mutated acute myeloid leukemia reveals prognostically-relevant features of the marrow microenvironment.
Modern Pathology ( IF 7.1 ) Pub Date : 2020-02-12 , DOI: 10.1038/s41379-020-0498-z Sanjay S Patel 1, 2 , Mikel Lipschitz 3 , Geraldine S Pinkus 2 , Jason L Weirather 3 , Olga Pozdnyakova 2 , Emily F Mason 4 , Giorgio Inghirami 1 , Robert P Hasserjian 5 , Scott J Rodig 2, 3 , Olga K Weinberg 2, 6
Modern Pathology ( IF 7.1 ) Pub Date : 2020-02-12 , DOI: 10.1038/s41379-020-0498-z Sanjay S Patel 1, 2 , Mikel Lipschitz 3 , Geraldine S Pinkus 2 , Jason L Weirather 3 , Olga Pozdnyakova 2 , Emily F Mason 4 , Giorgio Inghirami 1 , Robert P Hasserjian 5 , Scott J Rodig 2, 3 , Olga K Weinberg 2, 6
Affiliation
|
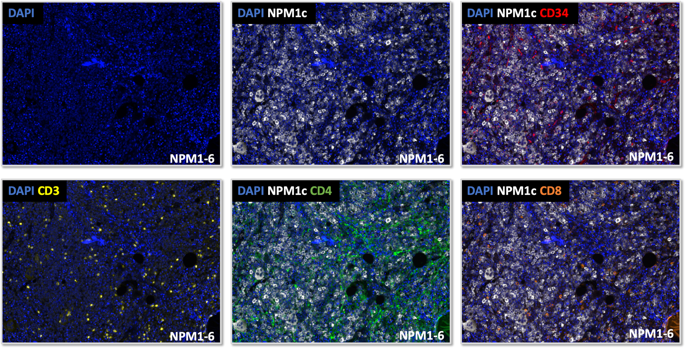
Ancillary testing during the initial workup of acute myeloid leukemia (AML) is largely performed using aspirated materials. We utilized multiplex immunofluorescence (MIF) imaging with digital image analysis to perform an in situ analysis of the microenvironment in NPM1-mutated AML using diagnostic bone marrow biopsy tissues (N = 17) and correlated these findings with diagnostic next-generation sequencing (NGS, N = 17), flow cytometry (FC, N = 14), and first remission (CR1) NPM1-specific molecular MRD (n = 16) data. The total CD3-positive T-cell percentages correlated positively between FC and MIF (r = 0.53, p = 0.05), but were significantly lower by MIF (1.62% vs. 3.4%, p = 0.009). The percentage of mutant NPM1-positive (NPM1c+) cells ranged from 9.7 to 90.8% (median 45.4%) and did not correlate with the NPM1 mutant allele fraction by NGS (p > 0.05). The percentage of CD34+/NPM1c+ cells ranged from 0 to 1.8% (median 0.07%). The percentage of NPM1c+ cells correlated inversely (34% vs. 62%, p = 0.03), while the percentages of CD3-/NPM1c- cells (64% vs. 35%, p = 0.03), and specifically CD3-/CD4-/NPM1c- cells (26% vs. 13%, p = 0.04), correlated positively with subsequent MRD. Discordances between MIF and FC/NGS data suggest that aspirate materials are likely an imperfect reflection of the core biopsy tissue. Furthermore, increased numbers of NPM1 wild-type cells within the microenvironment at diagnosis correlate with the subsequent presence of MRD.
中文翻译:

NPM1 突变的急性髓性白血病的多参数原位成像揭示了骨髓微环境的预后相关特征。
急性髓性白血病 (AML) 初始检查期间的辅助测试主要使用抽吸材料进行。我们利用多重免疫荧光 (MIF) 成像和数字图像分析,使用诊断性骨髓活检组织 (N = 17) 对 NPM1 突变 AML 中的微环境进行原位分析,并将这些发现与诊断性下一代测序 (NGS, N = 17)、流式细胞术(FC,N = 14)和首次缓解 (CR1) NPM1 特异性分子 MRD (n = 16) 数据。CD3 阳性 T 细胞总百分比在 FC 和 MIF 之间呈正相关(r = 0.53,p = 0.05),但 MIF 显着降低(1.62% 对 3.4%,p = 0.009)。突变 NPM1 阳性 (NPM1c+) 细胞的百分比范围为 9.7% 至 90.8%(中位数 45.4%),并且与 NGS 检测到的 NPM1 突变等位基因分数无关 (p > 0.05)。CD34+/NPM1c+ 细胞的百分比范围为 0 至 1.8%(中位数 0.07%)。NPM1c+ 细胞的百分比呈负相关(34% 对 62%,p = 0.03),而 CD3-/NPM1c- 细胞的百分比(64% 对 35%,p = 0.03),特别是 CD3-/CD4- /NPM1c- 细胞(26% 对 13%,p = 0.04)与随后的 MRD 呈正相关。MIF 和 FC/NGS 数据之间的不一致表明抽吸材料可能是核心活检组织的不完美反映。此外,诊断时微环境中 NPM1 野生型细胞数量的增加与随后出现的 MRD 相关。特别是 CD3-/CD4-/NPM1c- 细胞(26% 对 13%,p = 0.04),与随后的 MRD 呈正相关。MIF 和 FC/NGS 数据之间的不一致表明抽吸材料可能是核心活检组织的不完美反映。此外,诊断时微环境中 NPM1 野生型细胞数量的增加与随后出现的 MRD 相关。特别是 CD3-/CD4-/NPM1c- 细胞(26% 对 13%,p = 0.04),与随后的 MRD 呈正相关。MIF 和 FC/NGS 数据之间的不一致表明抽吸材料可能是核心活检组织的不完美反映。此外,诊断时微环境中 NPM1 野生型细胞数量的增加与随后出现的 MRD 相关。
更新日期:2020-02-13
中文翻译:

NPM1 突变的急性髓性白血病的多参数原位成像揭示了骨髓微环境的预后相关特征。
急性髓性白血病 (AML) 初始检查期间的辅助测试主要使用抽吸材料进行。我们利用多重免疫荧光 (MIF) 成像和数字图像分析,使用诊断性骨髓活检组织 (N = 17) 对 NPM1 突变 AML 中的微环境进行原位分析,并将这些发现与诊断性下一代测序 (NGS, N = 17)、流式细胞术(FC,N = 14)和首次缓解 (CR1) NPM1 特异性分子 MRD (n = 16) 数据。CD3 阳性 T 细胞总百分比在 FC 和 MIF 之间呈正相关(r = 0.53,p = 0.05),但 MIF 显着降低(1.62% 对 3.4%,p = 0.009)。突变 NPM1 阳性 (NPM1c+) 细胞的百分比范围为 9.7% 至 90.8%(中位数 45.4%),并且与 NGS 检测到的 NPM1 突变等位基因分数无关 (p > 0.05)。CD34+/NPM1c+ 细胞的百分比范围为 0 至 1.8%(中位数 0.07%)。NPM1c+ 细胞的百分比呈负相关(34% 对 62%,p = 0.03),而 CD3-/NPM1c- 细胞的百分比(64% 对 35%,p = 0.03),特别是 CD3-/CD4- /NPM1c- 细胞(26% 对 13%,p = 0.04)与随后的 MRD 呈正相关。MIF 和 FC/NGS 数据之间的不一致表明抽吸材料可能是核心活检组织的不完美反映。此外,诊断时微环境中 NPM1 野生型细胞数量的增加与随后出现的 MRD 相关。特别是 CD3-/CD4-/NPM1c- 细胞(26% 对 13%,p = 0.04),与随后的 MRD 呈正相关。MIF 和 FC/NGS 数据之间的不一致表明抽吸材料可能是核心活检组织的不完美反映。此外,诊断时微环境中 NPM1 野生型细胞数量的增加与随后出现的 MRD 相关。特别是 CD3-/CD4-/NPM1c- 细胞(26% 对 13%,p = 0.04),与随后的 MRD 呈正相关。MIF 和 FC/NGS 数据之间的不一致表明抽吸材料可能是核心活检组织的不完美反映。此外,诊断时微环境中 NPM1 野生型细胞数量的增加与随后出现的 MRD 相关。











































 京公网安备 11010802027423号
京公网安备 11010802027423号