Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
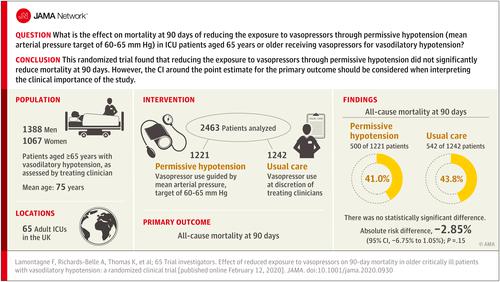
Effect of Reduced Exposure to Vasopressors on 90-Day Mortality in Older Critically Ill Patients With Vasodilatory Hypotension
JAMA ( IF 63.1 ) Pub Date : 2020-03-10 , DOI: 10.1001/jama.2020.0930 François Lamontagne 1, 2 , Alvin Richards-Belle 3 , Karen Thomas 3 , David A Harrison 3 , M Zia Sadique 4 , Richard D Grieve 4 , Julie Camsooksai 5 , Robert Darnell 3 , Anthony C Gordon 6, 7 , Doreen Henry 8 , Nicholas Hudson 3 , Alexina J Mason 4 , Michelle Saull 3 , Chris Whitman 8 , J Duncan Young 9 , Kathryn M Rowan 3 , Paul R Mouncey 3 ,
JAMA ( IF 63.1 ) Pub Date : 2020-03-10 , DOI: 10.1001/jama.2020.0930 François Lamontagne 1, 2 , Alvin Richards-Belle 3 , Karen Thomas 3 , David A Harrison 3 , M Zia Sadique 4 , Richard D Grieve 4 , Julie Camsooksai 5 , Robert Darnell 3 , Anthony C Gordon 6, 7 , Doreen Henry 8 , Nicholas Hudson 3 , Alexina J Mason 4 , Michelle Saull 3 , Chris Whitman 8 , J Duncan Young 9 , Kathryn M Rowan 3 , Paul R Mouncey 3 ,
Affiliation
|
Importance
Vasopressors are commonly administered to intensive care unit (ICU) patients to raise blood pressure. Balancing risks and benefits of vasopressors is a challenge, particularly in older patients. Objective
To determine whether reducing exposure to vasopressors through permissive hypotension (mean arterial pressure [MAP] target, 60-65 mm Hg) reduces mortality at 90 days in ICU patients aged 65 years or older with vasodilatory hypotension. Design, Setting, and Participants
A multicenter, pragmatic, randomized clinical trial was conducted in 65 ICUs in the United Kingdom and included 2600 randomized patients aged 65 years or older with vasodilatory hypotension (assessed by treating clinician). The study was conducted from July 2017 to March 2019, and follow-up was completed in August 2019. Interventions
Patients were randomized 1:1 to vasopressors guided either by MAP target (60-65 mm Hg, permissive hypotension) (n = 1291) or according to usual care (at the discretion of treating clinicians) (n = 1307). Main Outcome and Measures
The primary clinical outcome was all-cause mortality at 90 days. Results
Of 2600 randomized patients, after removal of those who declined or had withdrawn consent, 2463 (95%) were included in the analysis of the primary outcome (mean [SD] age 75 years [7 years]; 1387 [57%] men). Patients randomized to the permissive hypotension group had lower exposure to vasopressors compared with those in the usual care group (median duration 33 hours vs 38 hours; difference in medians, -5.0; 95% CI, -7.8 to -2.2 hours; total dose in norepinephrine equivalents median, 17.7 mg vs 26.4 mg; difference in medians, -8.7 mg; 95% CI, -12.8 to -4.6 mg). At 90 days, 500 of 1221 (41.0%) in the permissive hypotension compared with 544 of 1242 (43.8%) in the usual care group had died (absolute risk difference, -2.85%; 95% CI, -6.75 to 1.05; P = .15) (unadjusted relative risk, 0.93; 95% CI, 0.85-1.03). When adjusted for prespecified baseline variables, the odds ratio for 90-day mortality was 0.82 (95% CI, 0.68 to 0.98). Serious adverse events were reported for 79 patients (6.2%) in the permissive care group and 75 patients (5.8%) in the usual care group. The most common serious adverse events were acute renal failure (41 [3.2%] vs 33 [2.5%]) and supraventricular cardiac arrhythmia (12 [0.9%] vs 13 [1.0%]). Conclusions and Relevance
Among patients 65 years or older receiving vasopressors for vasodilatory hypotension, permissive hypotension compared with usual care did not result in a statistically significant reduction in mortality at 90 days. However, the confidence interval around the point estimate for the primary outcome should be considered when interpreting the clinical importance of the study. Trial Registration
isrctn.org Identifier: ISRCTN10580502.
中文翻译:

减少血管升压药暴露对老年危重血管舒张性低血压患者 90 天死亡率的影响
重要性 重症监护病房 (ICU) 患者通常使用血管加压药来升高血压。平衡血管加压药的风险和益处是一个挑战,特别是对于老年患者。目的 确定通过允许性低血压(平均动脉压 [MAP] 目标,60-65 mm Hg)减少血管加压药的暴露是否可以降低 65 岁或以上患有血管舒张性低血压的 ICU 患者 90 天时的死亡率。设计、环境和参与者 在英国 65 个 ICU 中进行了一项多中心、务实、随机临床试验,纳入了 2600 名 65 岁或以上患有血管舒张性低血压的随机患者(由治疗临床医生评估)。该研究于 2017 年 7 月至 2019 年 3 月进行,随访于 2019 年 8 月完成。 干预措施 患者按照 MAP 目标(60-65 mm Hg,允许性低血压)按 1:1 随机分配至血管加压药(n = 1291)或根据常规护理(由治疗临床医生决定)(n = 1307)。主要结果和措施 主要临床结果是 90 天的全因死亡率。结果 在 2600 名随机患者中,剔除那些拒绝或撤回同意的患者后,2463 名 (95%) 名患者被纳入主要结局分析(平均 [SD] 年龄 75 岁 [7 岁];1387 名 [57%] 男性)。与常规治疗组相比,随机分配到允许性低血压组的患者接受血管升压药的风险较低(中位持续时间 33 小时 vs 38 小时;中位差异,-5.0;95% CI,-7.8 至 -2.2 小时;总剂量去甲肾上腺素当量中位数,17.7 mg vs 26.4 mg;中位数差异,-8.7 mg;95% CI,-12.8 至 -4.6 mg)。 90 天时,1221 人中有 500 人(41.0%)患有允许性低血压,而 1242 人中有 544 人(43.0%)患有允许性低血压。常规护理组中 8%)死亡(绝对风险差异,-2.85%;95% CI,-6.75 至 1.05;P = .15)(未经调整的相对风险,0.93;95% CI,0.85-1.03)。根据预先指定的基线变量进行调整后,90 天死亡率的优势比为 0.82(95% CI,0.68 至 0.98)。宽容护理组有 79 名患者(6.2%)报告了严重不良事件,常规护理组有 75 名患者(5.8%)报告了严重不良事件。最常见的严重不良事件是急性肾衰竭(41例[3.2%] vs 33例[2.5%])和室上性心律失常(12例[0.9%] vs 13例[1.0%])。结论和相关性 在因血管舒张性低血压而接受血管升压药的 65 岁或以上患者中,与常规治疗相比,允许性低血压并未导致 90 天死亡率出现统计学上的显着降低。然而,在解释研究的临床重要性时,应考虑主要结果点估计的置信区间。试用注册 isrctn.org 标识符:ISRCTN10580502。
更新日期:2020-03-10
中文翻译:

减少血管升压药暴露对老年危重血管舒张性低血压患者 90 天死亡率的影响
重要性 重症监护病房 (ICU) 患者通常使用血管加压药来升高血压。平衡血管加压药的风险和益处是一个挑战,特别是对于老年患者。目的 确定通过允许性低血压(平均动脉压 [MAP] 目标,60-65 mm Hg)减少血管加压药的暴露是否可以降低 65 岁或以上患有血管舒张性低血压的 ICU 患者 90 天时的死亡率。设计、环境和参与者 在英国 65 个 ICU 中进行了一项多中心、务实、随机临床试验,纳入了 2600 名 65 岁或以上患有血管舒张性低血压的随机患者(由治疗临床医生评估)。该研究于 2017 年 7 月至 2019 年 3 月进行,随访于 2019 年 8 月完成。 干预措施 患者按照 MAP 目标(60-65 mm Hg,允许性低血压)按 1:1 随机分配至血管加压药(n = 1291)或根据常规护理(由治疗临床医生决定)(n = 1307)。主要结果和措施 主要临床结果是 90 天的全因死亡率。结果 在 2600 名随机患者中,剔除那些拒绝或撤回同意的患者后,2463 名 (95%) 名患者被纳入主要结局分析(平均 [SD] 年龄 75 岁 [7 岁];1387 名 [57%] 男性)。与常规治疗组相比,随机分配到允许性低血压组的患者接受血管升压药的风险较低(中位持续时间 33 小时 vs 38 小时;中位差异,-5.0;95% CI,-7.8 至 -2.2 小时;总剂量去甲肾上腺素当量中位数,17.7 mg vs 26.4 mg;中位数差异,-8.7 mg;95% CI,-12.8 至 -4.6 mg)。 90 天时,1221 人中有 500 人(41.0%)患有允许性低血压,而 1242 人中有 544 人(43.0%)患有允许性低血压。常规护理组中 8%)死亡(绝对风险差异,-2.85%;95% CI,-6.75 至 1.05;P = .15)(未经调整的相对风险,0.93;95% CI,0.85-1.03)。根据预先指定的基线变量进行调整后,90 天死亡率的优势比为 0.82(95% CI,0.68 至 0.98)。宽容护理组有 79 名患者(6.2%)报告了严重不良事件,常规护理组有 75 名患者(5.8%)报告了严重不良事件。最常见的严重不良事件是急性肾衰竭(41例[3.2%] vs 33例[2.5%])和室上性心律失常(12例[0.9%] vs 13例[1.0%])。结论和相关性 在因血管舒张性低血压而接受血管升压药的 65 岁或以上患者中,与常规治疗相比,允许性低血压并未导致 90 天死亡率出现统计学上的显着降低。然而,在解释研究的临床重要性时,应考虑主要结果点估计的置信区间。试用注册 isrctn.org 标识符:ISRCTN10580502。











































 京公网安备 11010802027423号
京公网安备 11010802027423号