当前位置:
X-MOL 学术
›
Hypertens. Res.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Mass clinical survey as a possible population strategy for the better control of hypertension in Japan
Hypertension Research ( IF 4.3 ) Pub Date : 2020-02-12 , DOI: 10.1038/s41440-019-0381-9 Kouichi Tamura 1 , Takahiro Yamaji 1 , Kengo Azushima 1, 2 , Hiromichi Wakui 1
Hypertension Research ( IF 4.3 ) Pub Date : 2020-02-12 , DOI: 10.1038/s41440-019-0381-9 Kouichi Tamura 1 , Takahiro Yamaji 1 , Kengo Azushima 1, 2 , Hiromichi Wakui 1
Affiliation
|
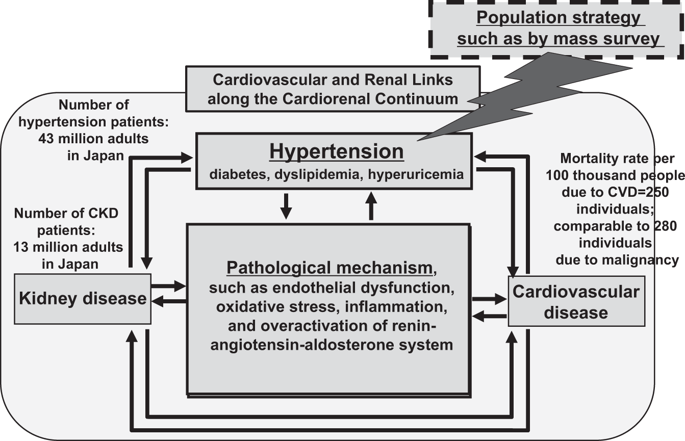
During the past century, human life expectancy has nearly doubled globally, increasing by more years than it did in all previous millennia combined [1]. Nevertheless, aging is a major risk factor for multiple noncommunicable diseases, such as cancers and cardiovascular, metabolic and neurodegenerative conditions, including hypertension and diabetes, which are the most common causes of premature death and morbidity. In addition, all of these pathological conditions require extensive long-term care and exert a critical impact on healthcare costs, productivity, and growth [1]. In particular, hypertension is one of the most pressing public health challenges. Hypertension is recognized as the biggest contributor to the global burden of disease [2]. Globally, in 2015, 1.13 billion adults had raised blood pressure (defined as a systolic blood pressure of 140 mmHg or higher or a diastolic blood pressure of 90 mmHg or higher) [3]. Hypertension is highly prevalent worldwide and is a major cause of strokes (such as cerebral infarction, cerebral hemorrhage, and subarachnoid hemorrhage), heart diseases (such as coronary artery disease, cardiac hypertrophy, and heart failure), kidney diseases (such as nephrosclerosis and end-stage kidney disease), and macrovascular diseases (such as aortic dissection and peripheral artery disease) [4]; thus, hypertension plays a key role in the progression of the pathological linkage between cardiovascular and kidney diseases (Fig. 1). Therefore, a primary aim of hypertension management is to present standard management strategies and evidence to all medical workers to provide appropriate treatment to patients with hypertension, most frequently encountered by clinicians/ practitioners in daily practice, for the prevention of the onset/progression of hypertension complications in the brain/heart/kidney by blood pressure control [5]. In Japan, a 2010 survey estimated that there were 43 million patients with hypertension, with only ~15–30% controlling their BP below 140/90 mmHg [6]. Because of the large number of individuals with hypertension and the poor control rate, hypertension is one of the leading causes of death (next to smoking) in Japan [7]. To improve hypertension management, a series of hypertension guidelines have been developed and updated regularly by various societies. For example, in recent years, overseas guidelines have been developed by the American College of Cardiology/American Heart Association and the European Society of Cardiology/European Society of Hypertension [8, 9]. These guidelines have created a considerable shift in the landscape of hypertension management [10]. In Japan, the Japanese Society of Hypertension (JSH) published its first guideline in 2000 (JSH 2000), which has been revised every 4 or 5 years, and the most updated version was released in April 2019 as the JSH Guidelines for the Management of Hypertension 2019 (JSH 2019) [11]. Even in the recently published JSH 2019 guidelines, only 50% of individuals are treated, and ~25% are controlled at a target BP level below 140/90 mmHg [11]. Concerning this important issue, several reasons were reported. For example, analyses using a Japanese claims database indicated that poor adherence to antihypertensive treatment was associated with a higher number of drugs and a higher number of pills prescribed [12]. Furthermore, physician problems, including the inappropriate use of antihypertensive drugs, are also involved in treatment resistance in many cases. The state in which medical workers, including physicians, do not comply with the necessity of enhancing antihypertensive treatment according to guidelines is termed “clinical inertia,” which is a great barrier to the achievement of target BP control in patients with hypertension [11]. * Kouichi Tamura tamukou@med.yokohama-cu.ac.jp
中文翻译:

大规模临床调查作为一种可能的人口策略,以更好地控制日本的高血压
在过去的一个世纪里,全球人类的预期寿命几乎翻了一番,增加的年数比之前所有千年的总和还要多 [1]。然而,衰老是多种非传染性疾病的主要风险因素,例如癌症和心血管、代谢和神经退行性疾病,包括高血压和糖尿病,这些都是过早死亡和发病的最常见原因。此外,所有这些病理状况都需要广泛的长期护理,并对医疗保健成本、生产力和增长产生关键影响 [1]。特别是,高血压是最紧迫的公共卫生挑战之一。高血压被认为是造成全球疾病负担的最大因素[2]。在全球范围内,2015 年,1。130 亿成年人血压升高(定义为收缩压 140 mmHg 或更高或舒张压 90 mmHg 或更高)[3]。高血压在世界范围内非常普遍,是中风(如脑梗塞、脑出血和蛛网膜下腔出血)、心脏病(如冠状动脉疾病、心脏肥大和心力衰竭)、肾脏疾病(如肾硬化和终末期肾病)和大血管疾病(如主动脉夹层和外周动脉疾病)[4];因此,高血压在心血管疾病和肾脏疾病之间病理联系的进展中起着关键作用(图1)。所以,高血压管理的一个主要目的是向所有医务人员提供标准的管理策略和证据,为临床医生/从业人员在日常实践中最常遇到的高血压患者提供适当的治疗,以预防高血压并发症的发生/进展。通过血压控制大脑/心脏/肾脏[5]。在日本,2010 年的一项调查估计有 4300 万高血压患者,只有约 15-30% 的人将他们的血压控制在 140/90 mmHg 以下 [6]。由于高血压患者人数众多且控制率低,高血压已成为日本(仅次于吸烟)的主要死亡原因之一[7]。为改善高血压管理,各学会制定并定期更新一系列高血压指南。例如,近年来,美国心脏病学会/美国心脏协会和欧洲心脏病学会/欧洲高血压学会制定了海外指南[8, 9]。这些指南使高血压管理领域发生了相当大的转变 [10]。在日本,日本高血压学会 (JSH) 于 2000 年发布了第一版指南 (JSH 2000),每 4 年或 5 年修订一次,最新版本于 2019 年 4 月发布为 JSH 管理指南。高血压 2019 (JSH 2019) [11]。即使在最近发布的 JSH 2019 指南中,也只有 50% 的人得到治疗,约 25% 的人被控制在低于 140/90 mmHg 的目标血压水平 [11]。关于这个重要问题,报告了几个原因。例如,使用日本索赔数据库的分析表明,抗高血压治疗依从性差与药物数量和处方药数量增加有关 [12]。此外,医生的问题,包括抗高血压药物的不当使用,在许多情况下也与治疗抵抗有关。包括医师在内的医务人员不遵守指导方针加强降压治疗的必要性被称为“临床惰性”,这是高血压患者实现目标血压控制的一大障碍[11]。* Kouichi Tamura tamukou@med.yokohama-cu.ac.jp 医生的问题,包括抗高血压药物的不当使用,在许多情况下也与治疗抵抗有关。包括医师在内的医务人员不遵守指导方针加强降压治疗的必要性被称为“临床惰性”,这是高血压患者实现目标血压控制的一大障碍[11]。* Kouichi Tamura tamukou@med.yokohama-cu.ac.jp 医生的问题,包括抗高血压药物的不当使用,在许多情况下也与治疗抵抗有关。包括医师在内的医务人员不遵守指导方针加强降压治疗的必要性被称为“临床惰性”,这是高血压患者实现目标血压控制的一大障碍[11]。* Kouichi Tamura tamukou@med.yokohama-cu.ac.jp ”,这是高血压患者实现目标血压控制的一大障碍[11]。* Kouichi Tamura tamukou@med.yokohama-cu.ac.jp ”,这是高血压患者实现目标血压控制的一大障碍[11]。* Kouichi Tamura tamukou@med.yokohama-cu.ac.jp
更新日期:2020-02-12
中文翻译:

大规模临床调查作为一种可能的人口策略,以更好地控制日本的高血压
在过去的一个世纪里,全球人类的预期寿命几乎翻了一番,增加的年数比之前所有千年的总和还要多 [1]。然而,衰老是多种非传染性疾病的主要风险因素,例如癌症和心血管、代谢和神经退行性疾病,包括高血压和糖尿病,这些都是过早死亡和发病的最常见原因。此外,所有这些病理状况都需要广泛的长期护理,并对医疗保健成本、生产力和增长产生关键影响 [1]。特别是,高血压是最紧迫的公共卫生挑战之一。高血压被认为是造成全球疾病负担的最大因素[2]。在全球范围内,2015 年,1。130 亿成年人血压升高(定义为收缩压 140 mmHg 或更高或舒张压 90 mmHg 或更高)[3]。高血压在世界范围内非常普遍,是中风(如脑梗塞、脑出血和蛛网膜下腔出血)、心脏病(如冠状动脉疾病、心脏肥大和心力衰竭)、肾脏疾病(如肾硬化和终末期肾病)和大血管疾病(如主动脉夹层和外周动脉疾病)[4];因此,高血压在心血管疾病和肾脏疾病之间病理联系的进展中起着关键作用(图1)。所以,高血压管理的一个主要目的是向所有医务人员提供标准的管理策略和证据,为临床医生/从业人员在日常实践中最常遇到的高血压患者提供适当的治疗,以预防高血压并发症的发生/进展。通过血压控制大脑/心脏/肾脏[5]。在日本,2010 年的一项调查估计有 4300 万高血压患者,只有约 15-30% 的人将他们的血压控制在 140/90 mmHg 以下 [6]。由于高血压患者人数众多且控制率低,高血压已成为日本(仅次于吸烟)的主要死亡原因之一[7]。为改善高血压管理,各学会制定并定期更新一系列高血压指南。例如,近年来,美国心脏病学会/美国心脏协会和欧洲心脏病学会/欧洲高血压学会制定了海外指南[8, 9]。这些指南使高血压管理领域发生了相当大的转变 [10]。在日本,日本高血压学会 (JSH) 于 2000 年发布了第一版指南 (JSH 2000),每 4 年或 5 年修订一次,最新版本于 2019 年 4 月发布为 JSH 管理指南。高血压 2019 (JSH 2019) [11]。即使在最近发布的 JSH 2019 指南中,也只有 50% 的人得到治疗,约 25% 的人被控制在低于 140/90 mmHg 的目标血压水平 [11]。关于这个重要问题,报告了几个原因。例如,使用日本索赔数据库的分析表明,抗高血压治疗依从性差与药物数量和处方药数量增加有关 [12]。此外,医生的问题,包括抗高血压药物的不当使用,在许多情况下也与治疗抵抗有关。包括医师在内的医务人员不遵守指导方针加强降压治疗的必要性被称为“临床惰性”,这是高血压患者实现目标血压控制的一大障碍[11]。* Kouichi Tamura tamukou@med.yokohama-cu.ac.jp 医生的问题,包括抗高血压药物的不当使用,在许多情况下也与治疗抵抗有关。包括医师在内的医务人员不遵守指导方针加强降压治疗的必要性被称为“临床惰性”,这是高血压患者实现目标血压控制的一大障碍[11]。* Kouichi Tamura tamukou@med.yokohama-cu.ac.jp 医生的问题,包括抗高血压药物的不当使用,在许多情况下也与治疗抵抗有关。包括医师在内的医务人员不遵守指导方针加强降压治疗的必要性被称为“临床惰性”,这是高血压患者实现目标血压控制的一大障碍[11]。* Kouichi Tamura tamukou@med.yokohama-cu.ac.jp ”,这是高血压患者实现目标血压控制的一大障碍[11]。* Kouichi Tamura tamukou@med.yokohama-cu.ac.jp ”,这是高血压患者实现目标血压控制的一大障碍[11]。* Kouichi Tamura tamukou@med.yokohama-cu.ac.jp











































 京公网安备 11010802027423号
京公网安备 11010802027423号