Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Association of Use of an Intravascular Microaxial Left Ventricular Assist Device vs Intra-aortic Balloon Pump With In-Hospital Mortality and Major Bleeding Among Patients With Acute Myocardial Infarction Complicated by Cardiogenic Shock
JAMA ( IF 63.1 ) Pub Date : 2020-02-25 , DOI: 10.1001/jama.2020.0254 Sanket S Dhruva 1, 2 , Joseph S Ross 3, 4, 5 , Bobak J Mortazavi 3, 6, 7, 8 , Nathan C Hurley 6 , Harlan M Krumholz 3, 5, 8 , Jeptha P Curtis 3, 8 , Alyssa Berkowitz 3 , Frederick A Masoudi 9 , John C Messenger 9 , Craig S Parzynski 3 , Che Ngufor 10, 11 , Saket Girotra 12 , Amit P Amin 13 , Nilay D Shah 10, 14 , Nihar R Desai 3, 8
JAMA ( IF 63.1 ) Pub Date : 2020-02-25 , DOI: 10.1001/jama.2020.0254 Sanket S Dhruva 1, 2 , Joseph S Ross 3, 4, 5 , Bobak J Mortazavi 3, 6, 7, 8 , Nathan C Hurley 6 , Harlan M Krumholz 3, 5, 8 , Jeptha P Curtis 3, 8 , Alyssa Berkowitz 3 , Frederick A Masoudi 9 , John C Messenger 9 , Craig S Parzynski 3 , Che Ngufor 10, 11 , Saket Girotra 12 , Amit P Amin 13 , Nilay D Shah 10, 14 , Nihar R Desai 3, 8
Affiliation
|
Importance
Acute myocardial infarction (AMI) complicated by cardiogenic shock is associated with substantial morbidity and mortality. Although intravascular microaxial left ventricular assist devices (LVADs) provide greater hemodynamic support as compared with intra-aortic balloon pumps (IABPs), little is known about clinical outcomes associated with intravascular microaxial LVAD use in clinical practice. Objective
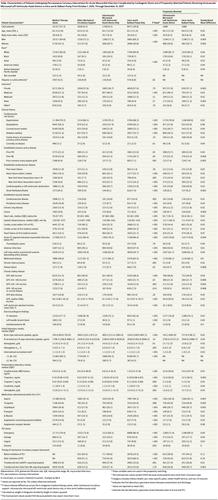
To examine outcomes among patients undergoing percutaneous coronary intervention (PCI) for AMI complicated by cardiogenic shock treated with mechanical circulatory support (MCS) devices. Design, Setting, and Participants
A propensity-matched registry-based retrospective cohort study of patients with AMI complicated by cardiogenic shock undergoing PCI between October 1, 2015, and December 31, 2017, who were included in data from hospitals participating in the CathPCI and the Chest Pain-MI registries, both part of the American College of Cardiology's National Cardiovascular Data Registry. Patients receiving an intravascular microaxial LVAD were matched with those receiving IABP on demographics, clinical history, presentation, infarct location, coronary anatomy, and clinical laboratory data, with final follow-up through December 31, 2017. Exposures
Hemodynamic support, categorized as intravascular microaxial LVAD use only, IABP only, other (such as use of a percutaneous extracorporeal ventricular assist system, extracorporeal membrane oxygenation, or a combination of MCS device use), or medical therapy only. Main Outcomes and Measures
The primary outcomes were in-hospital mortality and in-hospital major bleeding. Results
Among 28 304 patients undergoing PCI for AMI complicated by cardiogenic shock, the mean (SD) age was 65.0 (12.6) years, 67.0% were men, 81.3% had an ST-elevation myocardial infarction, and 43.3% had cardiac arrest. Over the study period among patients with AMI, an intravascular microaxial LVAD was used in 6.2% of patients, and IABP was used in 29.9%. Among 1680 propensity-matched pairs, there was a significantly higher risk of in-hospital death associated with use of an intravascular microaxial LVAD (45.0%) vs with an IABP (34.1% [absolute risk difference, 10.9 percentage points {95% CI, 7.6-14.2}; P < .001) and also higher risk of in-hospital major bleeding (intravascular microaxial LVAD [31.3%] vs IABP [16.0%]; absolute risk difference, 15.4 percentage points [95% CI, 12.5-18.2]; P < .001). These associations were consistent regardless of whether patients received a device before or after initiation of PCI. Conclusions and Relevance
Among patients undergoing PCI for AMI complicated by cardiogenic shock from 2015 to 2017, use of an intravascular microaxial LVAD compared with IABP was associated with higher adjusted risk of in-hospital death and major bleeding complications, although study interpretation is limited by the observational design. Further research may be needed to understand optimal device choice for these patients.
中文翻译:

急性心肌梗死并发心源性休克患者使用血管内微轴左心室辅助装置 vs 主动脉内球囊泵与院内死亡率和大出血的关联
重要性 急性心肌梗死 (AMI) 并发心源性休克与大量发病率和死亡率相关。尽管与主动脉内球囊泵 (IABP) 相比,血管内微轴左心室辅助装置 (LVAD) 可提供更好的血流动力学支持,但在临床实践中与血管内微轴 LVAD 使用相关的临床结果知之甚少。目的 探讨机械循环支持 (MCS) 装置治疗 AMI 并发心源性休克患者接受经皮冠状动脉介入治疗 (PCI) 的结果。设计、设置和参与者 一项基于倾向匹配注册的回顾性队列研究,研究对象为 2015 年 10 月 1 日至 2017 年 12 月 31 日期间接受 PCI 的 AMI 并发心源性休克患者,他们被纳入参与 CathPCI 和 Chest Pain-MI 注册的医院的数据中,这两个注册都是美国心脏病学会国家心血管数据注册的一部分。接受血管内微轴 LVAD 的患者与接受 IABP 的患者在人口统计学、临床病史、表现、梗死位置、冠状动脉解剖结构和临床实验室数据方面进行匹配,最终随访至 2017 年 12 月 31 日。 暴露 血液动力学支持,归类为血管内微轴仅使用 LVAD、仅使用 IABP、其他(例如使用经皮体外心室辅助系统、体外膜肺氧合或组合使用 MCS 设备)或仅药物治疗。主要结果和措施 主要结果是院内死亡率和院内大出血。结果28 304例AMI并发心源性休克行PCI的患者中,平均(SD)年龄为65.0(12.6)岁,67.0%为男性,81.3%为ST段抬高型心肌梗死,43.3%为心脏骤停。在 AMI 患者的研究期间,6.2% 的患者使用了血管内微轴 LVAD,29.9% 的患者使用了 IABP。在 1680 对倾向匹配的对中,与使用 IABP 相比,使用血管内微轴 LVAD (45.0%) 的院内死亡风险显着更高(34.1% [绝对风险差异,10.9 个百分点 {95% CI, 7.6-14.2};P < .001)以及院内大出血风险更高(血管内微轴 LVAD [31.3%] 与 IABP [16.0%];绝对风险差异,15.4 个百分点 [95% CI,12.5-18.2] ];P < .001)。无论患者在 PCI 开始之前还是之后接受了设备,这些关联都是一致的。结论和相关性 在 2015 年至 2017 年因 AMI 并发心源性休克而接受 PCI 的患者中,与 IABP 相比,使用血管内微轴 LVAD 与更高的院内死亡和大出血并发症的调整风险相关,尽管研究解释受到观察设计。可能需要进一步研究来了解这些患者的最佳设备选择。与 IABP 相比,使用血管内微轴 LVAD 与更高的院内死亡和大出血并发症的调整风险相关,尽管研究解释受到观察性设计的限制。可能需要进一步研究来了解这些患者的最佳设备选择。与 IABP 相比,使用血管内微轴 LVAD 与更高的院内死亡和大出血并发症的调整风险相关,尽管研究解释受到观察性设计的限制。可能需要进一步研究来了解这些患者的最佳设备选择。
更新日期:2020-02-25
中文翻译:

急性心肌梗死并发心源性休克患者使用血管内微轴左心室辅助装置 vs 主动脉内球囊泵与院内死亡率和大出血的关联
重要性 急性心肌梗死 (AMI) 并发心源性休克与大量发病率和死亡率相关。尽管与主动脉内球囊泵 (IABP) 相比,血管内微轴左心室辅助装置 (LVAD) 可提供更好的血流动力学支持,但在临床实践中与血管内微轴 LVAD 使用相关的临床结果知之甚少。目的 探讨机械循环支持 (MCS) 装置治疗 AMI 并发心源性休克患者接受经皮冠状动脉介入治疗 (PCI) 的结果。设计、设置和参与者 一项基于倾向匹配注册的回顾性队列研究,研究对象为 2015 年 10 月 1 日至 2017 年 12 月 31 日期间接受 PCI 的 AMI 并发心源性休克患者,他们被纳入参与 CathPCI 和 Chest Pain-MI 注册的医院的数据中,这两个注册都是美国心脏病学会国家心血管数据注册的一部分。接受血管内微轴 LVAD 的患者与接受 IABP 的患者在人口统计学、临床病史、表现、梗死位置、冠状动脉解剖结构和临床实验室数据方面进行匹配,最终随访至 2017 年 12 月 31 日。 暴露 血液动力学支持,归类为血管内微轴仅使用 LVAD、仅使用 IABP、其他(例如使用经皮体外心室辅助系统、体外膜肺氧合或组合使用 MCS 设备)或仅药物治疗。主要结果和措施 主要结果是院内死亡率和院内大出血。结果28 304例AMI并发心源性休克行PCI的患者中,平均(SD)年龄为65.0(12.6)岁,67.0%为男性,81.3%为ST段抬高型心肌梗死,43.3%为心脏骤停。在 AMI 患者的研究期间,6.2% 的患者使用了血管内微轴 LVAD,29.9% 的患者使用了 IABP。在 1680 对倾向匹配的对中,与使用 IABP 相比,使用血管内微轴 LVAD (45.0%) 的院内死亡风险显着更高(34.1% [绝对风险差异,10.9 个百分点 {95% CI, 7.6-14.2};P < .001)以及院内大出血风险更高(血管内微轴 LVAD [31.3%] 与 IABP [16.0%];绝对风险差异,15.4 个百分点 [95% CI,12.5-18.2] ];P < .001)。无论患者在 PCI 开始之前还是之后接受了设备,这些关联都是一致的。结论和相关性 在 2015 年至 2017 年因 AMI 并发心源性休克而接受 PCI 的患者中,与 IABP 相比,使用血管内微轴 LVAD 与更高的院内死亡和大出血并发症的调整风险相关,尽管研究解释受到观察设计。可能需要进一步研究来了解这些患者的最佳设备选择。与 IABP 相比,使用血管内微轴 LVAD 与更高的院内死亡和大出血并发症的调整风险相关,尽管研究解释受到观察性设计的限制。可能需要进一步研究来了解这些患者的最佳设备选择。与 IABP 相比,使用血管内微轴 LVAD 与更高的院内死亡和大出血并发症的调整风险相关,尽管研究解释受到观察性设计的限制。可能需要进一步研究来了解这些患者的最佳设备选择。









































 京公网安备 11010802027423号
京公网安备 11010802027423号