Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
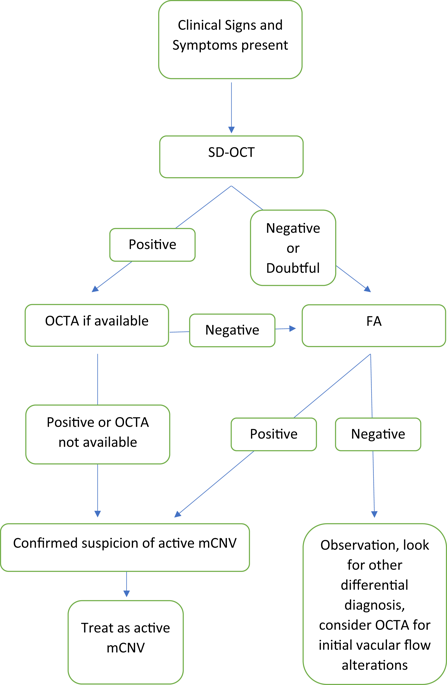
Comment on: Diagnostic algorithm utilising multimodal imaging including optical coherence tomography angiography for the detection of myopic choroidal neovascularization
Eye ( IF 2.8 ) Pub Date : 2020-02-06 , DOI: 10.1038/s41433-020-0787-2 Paolo Milani 1 , Fabrizio Scotti 1 , Fulvio Bergamini 1
Eye ( IF 2.8 ) Pub Date : 2020-02-06 , DOI: 10.1038/s41433-020-0787-2 Paolo Milani 1 , Fabrizio Scotti 1 , Fulvio Bergamini 1
Affiliation
|
Bagchi et al. [1] interestingly purposed a decision-making flow chart for cases clinically suspected of myopic choroidal neovascularization (mCNV) that may occasionally be misdiagnosed. In addition to an accurate clinical examination, diagnosis with complete multimodal imaging remains the best strategy because the sensitivity and specificity of spectral-domain optical coherence tomography (SD-OCT), optical coherence tomography angiography (OCTA), and fluorescein angiography (FA) alone is good but not infallible with a sensitivity ranging from 94 to 74% [1]. However, we believe that the flow chart warrants reconsideration for two main reasons. First, difficulty in determining the lesion activity clinically or on tomographic imaging. Some patients have reduced baseline visual acuity due to high myopia or concomitant diseases, such as amblyopia, cataract, and glaucoma. Therefore, these patients, especially those who are old, may be oblivious to further visual deterioration for months and may seek ophthalmologists’ care months after symptom onset when the mCNV is in the scar stage. Thus, non-invasive and fast SD-OCT to assess lesion characteristics becomes crucial, but in some eyes tomographic signs of activities, including the presence of hyperreflective material with intraretinal or subretinal fluid, intraretinal fuzzy area, and retinal pigment epithelium elevation, may be difficult to detect or dependent on the examiners’ interpretation and experience. Similarly, presence of ellipsoid zone and external limiting membrane interruption as signs of activity, as reported by some authors [2, 3], require additional validation and consensus since visual improvement and mCNV inactivity may occur after intravitreal treatment despite ellipsoid zone and external limiting membrane reconstitution within the lesion [4]. Occasionally, it is challenging to distinguish fibrosis from active mCNV on SDOCT. In such cases, OCTA may be potentially helpful, although there is a risk of false-negative diagnosis because of macular haemorrhage and chorioretinal atrophy. In fact, mCNV was identified on OCTA in 74.07% of cases by Bagchi et al. [1], concluding that the lesion shape (tight rather than a loose net) and presence of a black surrounding halo are the characteristic features of activity. In contrast, a low specificity of choroidal dark halo with no association with lesion activity was reported recently [5]. We therefore strongly believe that interpretation of mCNV features on OCTA is inter-observer dependent and that artifacts and acquisition modality can greatly affect diagnosis, eventually leading to poor quality imaging in almost 24.1% of cases [5]. Nevertheless, we reported that in 80% of fibrosis secondary to mCNV (inactive mCNV), the original neovascular network remains well discernable several months after treatment even if enclosed within the scar area [6]. This observation, in particular, seems inconsistent with the proposed algorithm. According to it, mCNV should be treated if considered negative on SD-OCT but positive on OCTA (as commonly seen with fibrosis or inactive mCNV) independently from its features on FA. Evidently, although SD-OCT is mostly sufficient for accurately diagnosing mCNV, we are convinced that FA should be strongly considered in mCNV cases with negative or doubtful SD-OCT outcomes, regardless of its invasiveness. In these cases, combined SD-OCT with OCTA, when available, may provide inaccurate diagnosis and lead to * Paolo Milani dottpaolomilani@hotmail.com
中文翻译:

评论:利用多模态成像(包括光学相干断层扫描血管造影)检测近视脉络膜新生血管的诊断算法
巴奇等人。[1] 有趣的是,针对临床上怀疑可能偶尔被误诊的近视脉络膜新生血管 (mCNV) 的病例制定了决策流程图。除了准确的临床检查外,完整的多模态成像诊断仍然是最佳策略,因为单独使用光谱域光学相干断层扫描 (SD-OCT)、光学相干断层扫描血管造影 (OCTA) 和荧光素血管造影 (FA) 的敏感性和特异性良好但并非绝对可靠,灵敏度范围为 94% 至 74% [1]。然而,我们认为流程图值得重新考虑,主要有两个原因。首先,在临床或断层成像上难以确定病变活动。一些患者由于高度近视或伴随疾病,如弱视,导致基线视力下降,白内障和青光眼。因此,这些患者,尤其是老年患者,可能会在数月内忘记视力进一步恶化,并且可能在 mCNV 处于瘢痕阶段时在症状出现数月后寻求眼科医生的护理。因此,评估病变特征的非侵入性和快速 SD-OCT 变得至关重要,但在某些眼睛的断层扫描迹象中,包括视网膜内或视网膜下液、视网膜内模糊区域和视网膜色素上皮升高的高反射物质的存在,可能是难以发现或取决于考官的解释和经验。类似地,正如一些作者 [2, 3] 所报告的,存在椭球区和外界膜中断作为活动的迹象,需要额外的验证和共识,因为玻璃体内治疗后可能会出现视力改善和 mCNV 不活动,尽管病灶内有椭球区和外界膜重建 [4]。有时,很难在 SDOCT 上区分纤维化和活跃的 mCNV。在这种情况下,OCTA 可能会有所帮助,尽管由于黄斑出血和脉络膜视网膜萎缩存在假阴性诊断的风险。事实上,Bagchi 等人 74.07% 的病例在 OCTA 上发现了 mCNV。[1],得出的结论是病变形状(紧密而不是松散的网状结构)和黑色周围光晕的存在是活动的特征。相比之下,最近报道了与病变活动无关的脉络膜暗晕的低特异性 [5]。因此,我们坚信 OCTA 上 mCNV 特征的解释依赖于观察者间,并且伪影和采集方式会极大地影响诊断,最终导致近 24.1% 的病例成像质量不佳 [5]。然而,我们报告说,在 80% 继发于 mCNV(非活动性 mCNV)的纤维化中,即使被封闭在疤痕区域内,原始的新生血管网络在治疗几个月后仍然可以很好地辨别 [6]。特别是这种观察似乎与所提出的算法不一致。根据它,如果 mCNV 在 SD-OCT 上被认为是阴性但在 OCTA 上被认为是阳性(如纤维化或非活动性 mCNV 中常见),则应独立于其在 FA 上的特征进行治疗。显然,虽然 SD-OCT 对准确诊断 mCNV 大多足够了,我们相信,无论其侵袭性如何,在 SD-OCT 结果为阴性或可疑的 mCNV 病例中都应强烈考虑 FA。在这些情况下,如果可用,将 SD-OCT 与 OCTA 结合使用可能会提供不准确的诊断并导致 * Paolo Milani dottpaolomilani@hotmail.com
更新日期:2020-02-06
中文翻译:

评论:利用多模态成像(包括光学相干断层扫描血管造影)检测近视脉络膜新生血管的诊断算法
巴奇等人。[1] 有趣的是,针对临床上怀疑可能偶尔被误诊的近视脉络膜新生血管 (mCNV) 的病例制定了决策流程图。除了准确的临床检查外,完整的多模态成像诊断仍然是最佳策略,因为单独使用光谱域光学相干断层扫描 (SD-OCT)、光学相干断层扫描血管造影 (OCTA) 和荧光素血管造影 (FA) 的敏感性和特异性良好但并非绝对可靠,灵敏度范围为 94% 至 74% [1]。然而,我们认为流程图值得重新考虑,主要有两个原因。首先,在临床或断层成像上难以确定病变活动。一些患者由于高度近视或伴随疾病,如弱视,导致基线视力下降,白内障和青光眼。因此,这些患者,尤其是老年患者,可能会在数月内忘记视力进一步恶化,并且可能在 mCNV 处于瘢痕阶段时在症状出现数月后寻求眼科医生的护理。因此,评估病变特征的非侵入性和快速 SD-OCT 变得至关重要,但在某些眼睛的断层扫描迹象中,包括视网膜内或视网膜下液、视网膜内模糊区域和视网膜色素上皮升高的高反射物质的存在,可能是难以发现或取决于考官的解释和经验。类似地,正如一些作者 [2, 3] 所报告的,存在椭球区和外界膜中断作为活动的迹象,需要额外的验证和共识,因为玻璃体内治疗后可能会出现视力改善和 mCNV 不活动,尽管病灶内有椭球区和外界膜重建 [4]。有时,很难在 SDOCT 上区分纤维化和活跃的 mCNV。在这种情况下,OCTA 可能会有所帮助,尽管由于黄斑出血和脉络膜视网膜萎缩存在假阴性诊断的风险。事实上,Bagchi 等人 74.07% 的病例在 OCTA 上发现了 mCNV。[1],得出的结论是病变形状(紧密而不是松散的网状结构)和黑色周围光晕的存在是活动的特征。相比之下,最近报道了与病变活动无关的脉络膜暗晕的低特异性 [5]。因此,我们坚信 OCTA 上 mCNV 特征的解释依赖于观察者间,并且伪影和采集方式会极大地影响诊断,最终导致近 24.1% 的病例成像质量不佳 [5]。然而,我们报告说,在 80% 继发于 mCNV(非活动性 mCNV)的纤维化中,即使被封闭在疤痕区域内,原始的新生血管网络在治疗几个月后仍然可以很好地辨别 [6]。特别是这种观察似乎与所提出的算法不一致。根据它,如果 mCNV 在 SD-OCT 上被认为是阴性但在 OCTA 上被认为是阳性(如纤维化或非活动性 mCNV 中常见),则应独立于其在 FA 上的特征进行治疗。显然,虽然 SD-OCT 对准确诊断 mCNV 大多足够了,我们相信,无论其侵袭性如何,在 SD-OCT 结果为阴性或可疑的 mCNV 病例中都应强烈考虑 FA。在这些情况下,如果可用,将 SD-OCT 与 OCTA 结合使用可能会提供不准确的诊断并导致 * Paolo Milani dottpaolomilani@hotmail.com











































 京公网安备 11010802027423号
京公网安备 11010802027423号