Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Impact of HPV vaccination and cervical screening on cervical cancer elimination: a comparative modelling analysis in 78 low-income and lower-middle-income countries.
The Lancet ( IF 98.4 ) Pub Date : 2020-01-30 , DOI: 10.1016/s0140-6736(20)30068-4 Marc Brisson 1 , Jane J Kim 2 , Karen Canfell 3 , Mélanie Drolet 4 , Guillaume Gingras 4 , Emily A Burger 5 , Dave Martin 4 , Kate T Simms 6 , Élodie Bénard 4 , Marie-Claude Boily 1 , Stephen Sy 2 , Catherine Regan 2 , Adam Keane 6 , Michael Caruana 6 , Diep T N Nguyen 6 , Megan A Smith 6 , Jean-François Laprise 4 , Mark Jit 7 , Michel Alary 8 , Freddie Bray 9 , Elena Fidarova 10 , Fayad Elsheikh 11 , Paul J N Bloem 11 , Nathalie Broutet 12 , Raymond Hutubessy 11
The Lancet ( IF 98.4 ) Pub Date : 2020-01-30 , DOI: 10.1016/s0140-6736(20)30068-4 Marc Brisson 1 , Jane J Kim 2 , Karen Canfell 3 , Mélanie Drolet 4 , Guillaume Gingras 4 , Emily A Burger 5 , Dave Martin 4 , Kate T Simms 6 , Élodie Bénard 4 , Marie-Claude Boily 1 , Stephen Sy 2 , Catherine Regan 2 , Adam Keane 6 , Michael Caruana 6 , Diep T N Nguyen 6 , Megan A Smith 6 , Jean-François Laprise 4 , Mark Jit 7 , Michel Alary 8 , Freddie Bray 9 , Elena Fidarova 10 , Fayad Elsheikh 11 , Paul J N Bloem 11 , Nathalie Broutet 12 , Raymond Hutubessy 11
Affiliation
|
BACKGROUND
The WHO Director-General has issued a call for action to eliminate cervical cancer as a public health problem. To help inform global efforts, we modelled potential human papillomavirus (HPV) vaccination and cervical screening scenarios in low-income and lower-middle-income countries (LMICs) to examine the feasibility and timing of elimination at different thresholds, and to estimate the number of cervical cancer cases averted on the path to elimination.
METHODS
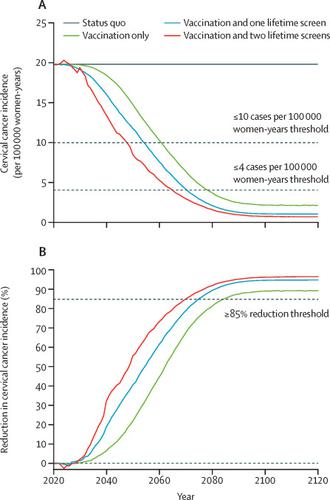
The WHO Cervical Cancer Elimination Modelling Consortium (CCEMC), which consists of three independent transmission-dynamic models identified by WHO according to predefined criteria, projected reductions in cervical cancer incidence over time in 78 LMICs for three standardised base-case scenarios: girls-only vaccination; girls-only vaccination and once-lifetime screening; and girls-only vaccination and twice-lifetime screening. Girls were vaccinated at age 9 years (with a catch-up to age 14 years), assuming 90% coverage and 100% lifetime protection against HPV types 16, 18, 31, 33, 45, 52, and 58. Cervical screening involved HPV testing once or twice per lifetime at ages 35 years and 45 years, with uptake increasing from 45% (2023) to 90% (2045 onwards). The elimination thresholds examined were an average age-standardised cervical cancer incidence of four or fewer cases per 100 000 women-years and ten or fewer cases per 100 000 women-years, and an 85% or greater reduction in incidence. Sensitivity analyses were done, varying vaccination and screening strategies and assumptions. We summarised results using the median (range) of model predictions.
FINDINGS
Girls-only HPV vaccination was predicted to reduce the median age-standardised cervical cancer incidence in LMICs from 19·8 (range 19·4-19·8) to 2·1 (2·0-2·6) cases per 100 000 women-years over the next century (89·4% [86·2-90·1] reduction), and to avert 61·0 million (60·5-63·0) cases during this period. Adding twice-lifetime screening reduced the incidence to 0·7 (0·6-1·6) cases per 100 000 women-years (96·7% [91·3-96·7] reduction) and averted an extra 12·1 million (9·5-13·7) cases. Girls-only vaccination was predicted to result in elimination in 60% (58-65) of LMICs based on the threshold of four or fewer cases per 100 000 women-years, in 99% (89-100) of LMICs based on the threshold of ten or fewer cases per 100 000 women-years, and in 87% (37-99) of LMICs based on the 85% or greater reduction threshold. When adding twice-lifetime screening, 100% (71-100) of LMICs reached elimination for all three thresholds. In regions in which all countries can achieve cervical cancer elimination with girls-only vaccination, elimination could occur between 2059 and 2102, depending on the threshold and region. Introducing twice-lifetime screening accelerated elimination by 11-31 years. Long-term vaccine protection was required for elimination.
INTERPRETATION
Predictions were consistent across our three models and suggest that high HPV vaccination coverage of girls can lead to cervical cancer elimination in most LMICs by the end of the century. Screening with high uptake will expedite reductions and will be necessary to eliminate cervical cancer in countries with the highest burden.
FUNDING
WHO, UNDP, UN Population Fund, UNICEF-WHO-World Bank Special Program of Research, Development and Research Training in Human Reproduction, Canadian Institute of Health Research, Fonds de recherche du Québec-Santé, Compute Canada, National Health and Medical Research Council Australia Centre for Research Excellence in Cervical Cancer Control.
中文翻译:

HPV 疫苗接种和宫颈筛查对消除宫颈癌的影响:78 个低收入和中低收入国家的比较模型分析。
背景 WHO 总干事已发出呼吁,要求采取行动消除宫颈癌这一公共卫生问题。为了帮助为全球努力提供信息,我们模拟了低收入和中低收入国家 (LMIC) 的潜在人乳头瘤病毒 (HPV) 疫苗接种和宫颈筛查方案,以检查在不同阈值下消除的可行性和时间,并估计数量宫颈癌病例在消除道路上得以避免。方法 WHO 宫颈癌消除模型联合会 (CCEMC) 由 WHO 根据预先定义的标准确定的三个独立的传播动态模型组成,针对三个标准化的基本案例情景,预测 78 个 LMICs 的宫颈癌发病率随着时间的推移会减少:女孩 -仅接种疫苗;仅限女孩的疫苗接种和终身筛查;以及仅限女孩的疫苗接种和两次终生筛查。女孩在 9 岁时接种疫苗(追赶到 14 岁),假设 90% 的覆盖率和 100% 的终生保护针对 HPV 类型 16、18、31、33、45、52 和 58。宫颈筛查涉及 HPV在 35 岁和 45 岁的人一生中检测一次或两次,接受率从 45%(2023 年)增加到 90%(2045 年起)。检查的消除阈值是平均年龄标准化宫颈癌发病率为每 100 000 名女性年 4 例或更少,每 100 000 名女性年 10 例或更少,并且发病率降低 85% 或更多。进行了敏感性分析,改变了疫苗接种和筛查策略和假设。我们使用模型预测的中值(范围)总结了结果。调查结果 预计仅女孩接种 HPV 疫苗可将中低收入国家的年龄标准化宫颈癌中位发病率从每 100 人 19·8(范围 19·4-19·8)降至 2·1(2·0-2·6)例下个世纪 000 名妇女年(减少 89·4% [86·2-90·1]),并在此期间避免 61·0 万 (60·5-63·0) 例。增加两次终生筛查可将发病率降低至每 100 000 名女性年 0·7 (0·6-1·6) 例(减少 96·7% [91·3-96·7])并避免额外的 12· 100万(9·5-13·7)例。根据每 100 000 名妇女年 4 例或更少病例的阈值,预计 60%(58-65)的 LMIC 会消除 60%(58-65)的仅女孩接种疫苗,根据阈值,99%(89-100)的 LMIC 会消除每 100 000 名女性每年 10 例或更少的病例数,以及 87% (37-99) 的中低收入国家(基于 85% 或更高的减少阈值)。当添加两次终生筛查时,100% (71-100) 的 LMIC 达到了所有三个阈值的消除。在所有国家都可以通过仅对女孩进行疫苗接种来消除宫颈癌的地区,根据阈值和地区的不同,可能会在 2059 年至 2102 年之间实现消除。引入两次终生筛选可加速 11-31 岁的淘汰。消除需要长期的疫苗保护。解释 我们的三个模型的预测是一致的,表明到本世纪末,女孩的 HPV 疫苗接种率高可以导致大多数 LMIC 消除宫颈癌。接受率高的筛查将加快减少,并且对于消除负担最重的国家的宫颈癌是必要的。资金 世卫组织、开发计划署、联合国人口基金,
更新日期:2020-02-21
中文翻译:

HPV 疫苗接种和宫颈筛查对消除宫颈癌的影响:78 个低收入和中低收入国家的比较模型分析。
背景 WHO 总干事已发出呼吁,要求采取行动消除宫颈癌这一公共卫生问题。为了帮助为全球努力提供信息,我们模拟了低收入和中低收入国家 (LMIC) 的潜在人乳头瘤病毒 (HPV) 疫苗接种和宫颈筛查方案,以检查在不同阈值下消除的可行性和时间,并估计数量宫颈癌病例在消除道路上得以避免。方法 WHO 宫颈癌消除模型联合会 (CCEMC) 由 WHO 根据预先定义的标准确定的三个独立的传播动态模型组成,针对三个标准化的基本案例情景,预测 78 个 LMICs 的宫颈癌发病率随着时间的推移会减少:女孩 -仅接种疫苗;仅限女孩的疫苗接种和终身筛查;以及仅限女孩的疫苗接种和两次终生筛查。女孩在 9 岁时接种疫苗(追赶到 14 岁),假设 90% 的覆盖率和 100% 的终生保护针对 HPV 类型 16、18、31、33、45、52 和 58。宫颈筛查涉及 HPV在 35 岁和 45 岁的人一生中检测一次或两次,接受率从 45%(2023 年)增加到 90%(2045 年起)。检查的消除阈值是平均年龄标准化宫颈癌发病率为每 100 000 名女性年 4 例或更少,每 100 000 名女性年 10 例或更少,并且发病率降低 85% 或更多。进行了敏感性分析,改变了疫苗接种和筛查策略和假设。我们使用模型预测的中值(范围)总结了结果。调查结果 预计仅女孩接种 HPV 疫苗可将中低收入国家的年龄标准化宫颈癌中位发病率从每 100 人 19·8(范围 19·4-19·8)降至 2·1(2·0-2·6)例下个世纪 000 名妇女年(减少 89·4% [86·2-90·1]),并在此期间避免 61·0 万 (60·5-63·0) 例。增加两次终生筛查可将发病率降低至每 100 000 名女性年 0·7 (0·6-1·6) 例(减少 96·7% [91·3-96·7])并避免额外的 12· 100万(9·5-13·7)例。根据每 100 000 名妇女年 4 例或更少病例的阈值,预计 60%(58-65)的 LMIC 会消除 60%(58-65)的仅女孩接种疫苗,根据阈值,99%(89-100)的 LMIC 会消除每 100 000 名女性每年 10 例或更少的病例数,以及 87% (37-99) 的中低收入国家(基于 85% 或更高的减少阈值)。当添加两次终生筛查时,100% (71-100) 的 LMIC 达到了所有三个阈值的消除。在所有国家都可以通过仅对女孩进行疫苗接种来消除宫颈癌的地区,根据阈值和地区的不同,可能会在 2059 年至 2102 年之间实现消除。引入两次终生筛选可加速 11-31 岁的淘汰。消除需要长期的疫苗保护。解释 我们的三个模型的预测是一致的,表明到本世纪末,女孩的 HPV 疫苗接种率高可以导致大多数 LMIC 消除宫颈癌。接受率高的筛查将加快减少,并且对于消除负担最重的国家的宫颈癌是必要的。资金 世卫组织、开发计划署、联合国人口基金,











































 京公网安备 11010802027423号
京公网安备 11010802027423号