当前位置:
X-MOL 学术
›
JAMA Neurol.
›
论文详情
Our official English website, www.x-mol.net, welcomes your
feedback! (Note: you will need to create a separate account there.)
Blood Pressure Thresholds and Neurologic Outcomes After Endovascular Therapy for Acute Ischemic Stroke: An Analysis of Individual Patient Data From 3 Randomized Clinical Trials.
JAMA Neurology ( IF 20.4 ) Pub Date : 2020-05-01 , DOI: 10.1001/jamaneurol.2019.4838 Mads Rasmussen 1 , Silvia Schönenberger 2 , Pia Löwhagen Hendèn 3 , Jan B Valentin 4 , Ulrick S Espelund 5 , Leif H Sørensen 6 , Niels Juul 1 , Lorenz Uhlmann 7 , Søren P Johnsen 4 , Alexandros Rentzos 8 , Julian Bösel 9 , Claus Z Simonsen 10 ,
JAMA Neurology ( IF 20.4 ) Pub Date : 2020-05-01 , DOI: 10.1001/jamaneurol.2019.4838 Mads Rasmussen 1 , Silvia Schönenberger 2 , Pia Löwhagen Hendèn 3 , Jan B Valentin 4 , Ulrick S Espelund 5 , Leif H Sørensen 6 , Niels Juul 1 , Lorenz Uhlmann 7 , Søren P Johnsen 4 , Alexandros Rentzos 8 , Julian Bösel 9 , Claus Z Simonsen 10 ,
Affiliation
|
Importance
The optimal blood pressure targets during endovascular therapy (EVT) for acute ischemic stroke (AIS) are unknown.
Objective
To study whether procedural blood pressure parameters, including specific blood pressure thresholds, are associated with neurologic outcomes after EVT.
Design, Setting, and Participants
This retrospective cohort study included adults with anterior-circulation AIS who were enrolled in randomized clinical trials assessing anesthetic strategy for EVT between February 2014 and February 2017. The trials had comparable blood pressure protocols, and patients were followed up for 90 days. A total of 3630 patients were initially approached, and 3265 patients were excluded.
Exposure
Endovascular therapy.
Main Outcomes and Measures
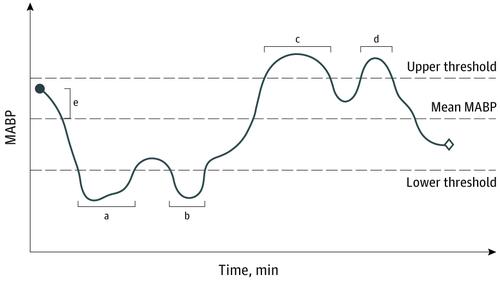
The primary efficacy variable was functional outcome as defined by the modified Rankin Scale (mRS) score at 90 days. Associations of blood pressure parameters and time less than and greater than mean arterial blood pressure (MABP) thresholds with outcome were analyzed.
Results
Of the 365 patients included in the analysis, the mean (SD) age was 71.4 (13.0) years, 163 were women (44.6%), and the median National Institutes of Health Stroke Scale score was 17 (interquartile range [IQR], 14-21). For the entire cohort, 182 (49.9%) received general anesthesia and 183 (50.1%) received procedural sedation. A cumulated period of minimum 10 minutes with less than 70 mm Hg MABP (adjusted OR, 1.51; 95% CI, 1.02-2.22) and a continuous episode of minimum 20 minutes with less than 70 mm Hg MABP (adjusted OR, 2.30; 95% CI, 1.11-4.75) were associated with a shift toward higher 90-day mRS scores, corresponding to a number needed to harm of 10 and 4, respectively. A cumulated period of minimum 45 minutes with greater than 90 mm Hg MABP (adjusted OR, 1.49; 95% CI, 1.11-2.02) and a continuous episode of minimum 115 minutes with greater than 90 mm Hg MABP (adjusted OR, 1.89; 95% CI, 1.01-3.54) were associated with a shift toward higher 90-day mRS scores, corresponding to a number needed to harm of 10 and 6, respectively.
Conclusions and Relevance
Critical MABP thresholds and durations for poor outcome were found to be MABP less than 70 mm Hg for more than 10 minutes and MABP greater than 90 mm Hg for more than 45 minutes, both durations with a number needed to harm of 10 patients. Mean arterial blood pressure may be a modifiable therapeutic target to prevent or reduce poor functional outcome after EVT.
中文翻译:

急性缺血性卒中的血管内治疗后的血压阈值和神经系统结果:来自3个随机临床试验的患者个人数据分析。
重要性急性缺血性卒中(AIS)的血管内治疗(EVT)期间的最佳血压目标尚不清楚。目的研究程序性血压参数(包括特定血压阈值)是否与EVT后的神经系统结果相关。设计,设置和参加者这项回顾性队列研究包括2014年2月至2017年2月之间参加评估EVT麻醉策略的随机临床试验的成年前AIS成人。 90天。最初共有3630名患者进入研究,其中3265名患者被排除在外。暴露血管内治疗。主要结果和措施主要疗效变量是功能结果,如90天时的改良Rankin量表(mRS)评分所定义。分析了血压参数和小于和大于平均动脉血压(MABP)阈值的时间与预后的关系。结果分析的365名患者中,平均(SD)年龄为71.4(13.0)岁,女性(163)为女性(44.6%),美国国立卫生研究院卒中量表评分中位数为17(四分位数范围[IQR], 14-21)。在整个队列中,有182例(49.9%)接受了全身麻醉,而183例(50.1%)接受了手术镇静。累积最少10分钟的时间少于70毫米汞柱MABP(调整后的OR,1.51; 95%CI,1.02-2.22)和连续发作最少20分钟的连续时间少于20毫米汞柱MABP(调整的OR,2.30; 95 %CI,1.11-4。75)与迈向更高的90天mRS分数相关,分别对应于伤害10和4所需的数字。大于45毫米汞柱MABP的最小累积时间为45分钟(调整后的OR,1.49; 95%CI,1.11-2.02),大于90毫米汞柱MABP的最小持续时间至少为115分钟(调整后的OR,1.89; 95 %CI,1.01-3.54)与向更高的90天mRS得分过渡有关,分别对应于伤害10和6所需的数字。结论和相关性发现不良结果的关键MABP阈值和持续时间为MABP小于70 mm Hg持续10分钟以上,MABP大于90 mm Hg持续45分钟以上,两种持续时间都需要伤害10位患者。
更新日期:2020-05-01
中文翻译:

急性缺血性卒中的血管内治疗后的血压阈值和神经系统结果:来自3个随机临床试验的患者个人数据分析。
重要性急性缺血性卒中(AIS)的血管内治疗(EVT)期间的最佳血压目标尚不清楚。目的研究程序性血压参数(包括特定血压阈值)是否与EVT后的神经系统结果相关。设计,设置和参加者这项回顾性队列研究包括2014年2月至2017年2月之间参加评估EVT麻醉策略的随机临床试验的成年前AIS成人。 90天。最初共有3630名患者进入研究,其中3265名患者被排除在外。暴露血管内治疗。主要结果和措施主要疗效变量是功能结果,如90天时的改良Rankin量表(mRS)评分所定义。分析了血压参数和小于和大于平均动脉血压(MABP)阈值的时间与预后的关系。结果分析的365名患者中,平均(SD)年龄为71.4(13.0)岁,女性(163)为女性(44.6%),美国国立卫生研究院卒中量表评分中位数为17(四分位数范围[IQR], 14-21)。在整个队列中,有182例(49.9%)接受了全身麻醉,而183例(50.1%)接受了手术镇静。累积最少10分钟的时间少于70毫米汞柱MABP(调整后的OR,1.51; 95%CI,1.02-2.22)和连续发作最少20分钟的连续时间少于20毫米汞柱MABP(调整的OR,2.30; 95 %CI,1.11-4。75)与迈向更高的90天mRS分数相关,分别对应于伤害10和4所需的数字。大于45毫米汞柱MABP的最小累积时间为45分钟(调整后的OR,1.49; 95%CI,1.11-2.02),大于90毫米汞柱MABP的最小持续时间至少为115分钟(调整后的OR,1.89; 95 %CI,1.01-3.54)与向更高的90天mRS得分过渡有关,分别对应于伤害10和6所需的数字。结论和相关性发现不良结果的关键MABP阈值和持续时间为MABP小于70 mm Hg持续10分钟以上,MABP大于90 mm Hg持续45分钟以上,两种持续时间都需要伤害10位患者。











































 京公网安备 11010802027423号
京公网安备 11010802027423号